Most people don’t feel high cholesterol until it’s too late. There’s no pain, no warning sign, no sudden jolt-just silent buildup in your arteries, quietly narrowing the pathways your heart depends on. By the time chest pain or a heart attack hits, the damage is often already advanced. That’s why understanding hypercholesterolemia isn’t just about numbers on a lab report-it’s about survival.
What Exactly Is Hypercholesterolemia?
Hypercholesterolemia simply means too much cholesterol in your blood. Cholesterol itself isn’t bad. Your body needs it to build cells, make hormones, and digest food. But when levels climb too high-especially the bad kind, called LDL (low-density lipoprotein)-it starts sticking to artery walls. Over time, this creates plaque. Plaque hardens, narrows arteries, and can suddenly block blood flow. That’s when heart attacks and strokes happen.
The American Heart Association says about 93 million American adults have total cholesterol over 200 mg/dL. In the UK, NHS data shows similar trends: nearly half of adults over 45 have elevated cholesterol. The real danger? Most of them don’t know it.
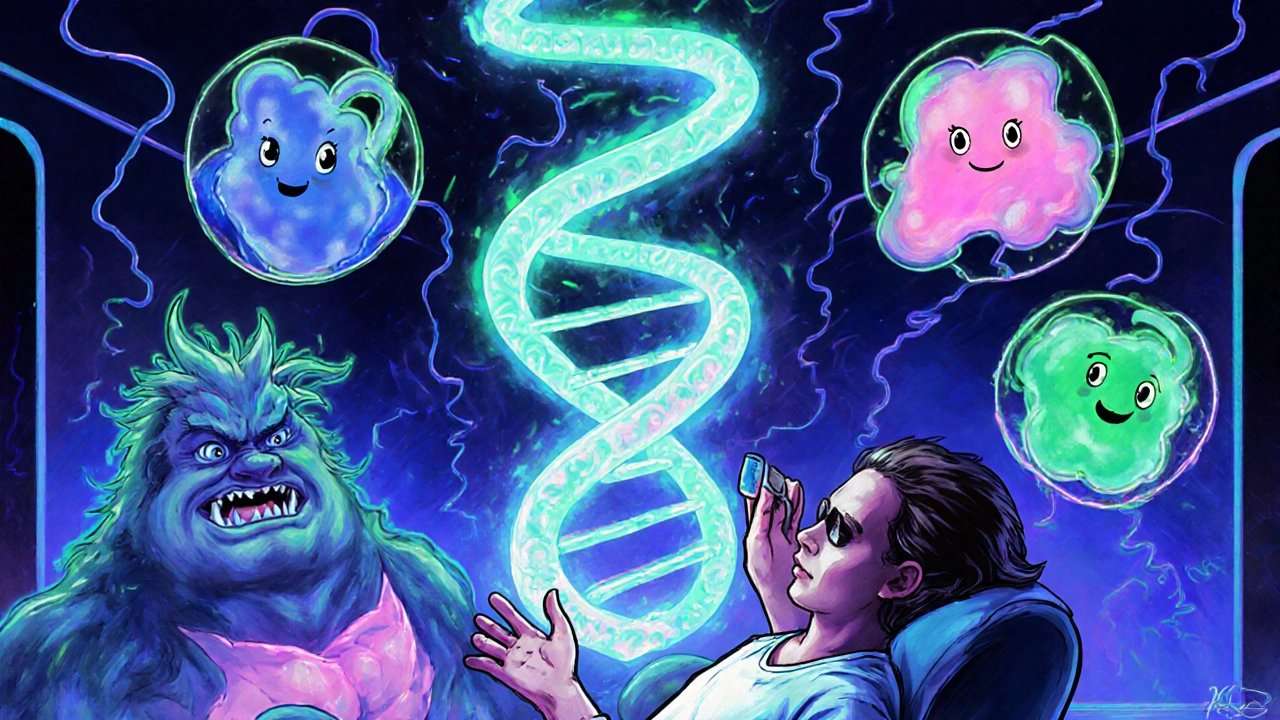
Familial vs. Acquired: Two Very Different Causes
Not all high cholesterol is the same. There are two main types: inherited (familial) and lifestyle-driven (acquired).
Familial hypercholesterolemia (FH) is genetic. You’re born with it. One faulty gene-usually in the LDLR or PCSK9 gene-means your body can’t clear LDL from your blood properly. This isn’t rare. About 1 in 250 people globally have heterozygous FH. In the UK, that’s around 250,000 people. Many never get diagnosed.
People with FH often have LDL levels above 190 mg/dL from childhood. By age 30, you might see fatty lumps on tendons-especially the Achilles or knuckles. These are called tendon xanthomas. Yellowish patches around the eyelids? That’s xanthelasmas. Both are red flags for FH.
Without treatment, men with FH have a 50% chance of a heart attack by age 50. Women aren’t much safer-risk spikes by 60. Homozygous FH? That’s even worse. LDL can hit 450 mg/dL or higher. Heart attacks before age 20 aren’t unheard of.
Then there’s acquired hypercholesterolemia. This is the kind tied to diet, weight, and other health issues. Think: too many fried foods, sugary drinks, lack of movement, or conditions like diabetes, hypothyroidism, or kidney disease. These cases usually have LDL under 190 mg/dL and respond better to lifestyle changes.
How Do You Know If You Have It?
There are no symptoms. Not until something breaks.
The only way to know is a simple blood test-a lipid panel. You don’t even need to fast anymore. The National Lipid Association confirmed in 2021 that non-fasting tests are just as accurate for screening. Most doctors will check cholesterol during routine visits after age 40, but if you have a family history of early heart disease, get tested earlier-even in your 20s.
Here’s what the numbers mean:
- Total cholesterol: Under 200 mg/dL is ideal
- LDL (bad cholesterol): Under 100 mg/dL is best; under 70 if you’ve had a heart event
- HDL (good cholesterol): Above 60 mg/dL is protective
- Triglycerides: Under 150 mg/dL
Levels above 190 mg/dL for LDL? That’s a red flag for FH. Between 130-159? You’re at elevated risk if you smoke, have high blood pressure, or are overweight.
Why Statins Are Still the First Line of Defense
If your LDL is too high, your doctor will likely start you on a statin. These drugs block cholesterol production in the liver. Simple. Effective. Proven.
High-intensity statins-like atorvastatin (40-80 mg) or rosuvastatin (20-40 mg)-can slash LDL by 50% or more. That’s not just a number. It’s a life saved. The IMPROVE-IT trial showed that for every 39 mg/dL drop in LDL, your risk of heart attack or stroke drops by 22%.
But not everyone tolerates statins. About 7-29% of people report muscle pain or fatigue. That doesn’t always mean you can’t take them-sometimes it’s just a dose issue. But if you truly can’t, alternatives exist.
Ezetimibe reduces cholesterol absorption in the gut. It lowers LDL by about 18%. It’s often added to statins for extra punch. Then there’s PCSK9 inhibitors-injectables like alirocumab and evolocumab. These can drop LDL another 50-60% on top of statins. They’re expensive, but for FH patients, they’re often essential.
And now there’s inclisiran (Leqvio). Approved in 2021, it’s a twice-yearly injection that silences the gene responsible for making PCSK9. It cuts LDL by half, with minimal side effects. It’s a game-changer for people who struggle with daily pills.
Lifestyle Changes: Do They Really Work?
Yes-but only if you stick with them.
The Portfolio Diet, studied in JAMA Cardiology, combines plant sterols, oats, nuts, soy, and fiber. In trials, it lowered LDL by 30%-as much as a low-dose statin. But here’s the catch: only 45% of people kept it up after a year. That’s the problem. It’s hard to change lifelong habits.
What actually works?
- Swap butter for olive oil
- Choose whole grains over white bread
- Eat beans, lentils, and chickpeas daily
- Snack on almonds or walnuts (a small handful)
- Avoid processed meats, fried foods, and sugary cereals
And exercise? It doesn’t lower LDL much-but it raises HDL (good cholesterol) and helps control weight and blood pressure. Aim for 150 minutes a week. Walk. Cycle. Dance. Just move.
For FH patients, diet alone won’t cut it. But for acquired high cholesterol, lifestyle changes can be enough-especially if caught early.
Who’s Getting Left Behind?
Even with all the tools available, many people aren’t getting treated.
NHANES data shows only 55.5% of U.S. adults with high cholesterol are on statins. Among Black adults, it’s 42.3%. In the UK, NHS figures show only 48% of high-risk patients hit their LDL targets. Why?
- Doctors don’t always test high-risk groups early enough
- Patients stop meds because they feel fine
- Cost and access block newer treatments like PCSK9 inhibitors
- There’s still confusion about dietary cholesterol
Here’s the myth: “Eating eggs raises your cholesterol.” The Dietary Guidelines for Americans removed the 300 mg/day limit in 2020 because research shows dietary cholesterol has less impact than saturated and trans fats. But a 2019 JAMA study found that every extra 300 mg of cholesterol eaten per day (about two eggs) raised heart disease risk by 17%. So it’s not black and white.
The real villain? Saturated fat-found in fatty meats, full-fat dairy, and baked goods. That’s what pushes LDL up. Cut that, and you cut risk.
What’s Next? The Future of Cholesterol Management
The field is moving fast.
Polygenic risk scores-analyzing dozens of small genetic variants-are now used to identify people with “polygenic hypercholesterolemia.” These aren’t FH patients, but their cholesterol is still high due to combined small genetic hits. They need earlier intervention than we used to think.
Also, obesity is rising. By 2030, half of U.S. adults could be obese. That means more secondary hypercholesterolemia from insulin resistance and fatty liver disease. Prevention will need to target diet and activity at the population level.
The American Heart Association’s 2030 goal? A 20% improvement in heart health metrics-including cholesterol control-through better screening, digital health tools, and policy changes like taxing sugary drinks and limiting trans fats in food.
What Should You Do Now?
Don’t wait for symptoms. Don’t assume you’re fine because you feel okay.
- If you’re over 40, ask for a lipid panel at your next checkup.
- If you have a family history of early heart disease (before 55 for men, 65 for women), get tested in your 20s or 30s.
- If your LDL is above 190, push for genetic testing for FH.
- If you’re on statins, don’t stop just because you feel fine.
- If you’re not on meds, start with diet and movement. Give it 3 months. Then retest.
High cholesterol isn’t a life sentence. It’s a signal. And with the right steps-testing, treatment, and consistent habits-you can live just as long as someone with normal levels.
Can high cholesterol be reversed without medication?
Yes-for many people, especially those with lifestyle-driven high cholesterol. The Portfolio Diet, regular exercise, and losing excess weight can lower LDL by 20-30%. But if your LDL is above 190 mg/dL, or you have a family history of early heart disease, diet alone usually isn’t enough. Genetic forms like familial hypercholesterolemia require medication to reach safe levels.
Is familial hypercholesterolemia common?
Yes. About 1 in 250 people have heterozygous familial hypercholesterolemia (FH), meaning roughly 250,000 people in the UK alone. But fewer than 10% are diagnosed. It’s under-recognized because it has no symptoms until a heart event occurs. If a parent or sibling had a heart attack before age 55, get tested.
Do I need to fast before a cholesterol test?
No. Since 2021, major guidelines like those from the National Lipid Association confirm that non-fasting lipid panels are accurate for screening. You can eat and drink normally before the test. Fasting is only required if your doctor needs to check triglycerides in detail-for example, if levels are very high.
What are the side effects of statins?
The most common side effect is mild muscle soreness or fatigue, affecting 7-29% of users. Serious muscle damage (rhabdomyolysis) is extremely rare-less than 1 in 10,000. Other side effects include a slight increase in blood sugar, which may slightly raise diabetes risk in predisposed people. But the benefit of preventing heart attacks far outweighs these risks for most.
Can I stop taking cholesterol meds if my levels improve?
Not usually. Cholesterol meds don’t cure the problem-they manage it. If you stop, your levels will likely rise again. For familial hypercholesterolemia, you’ll need lifelong treatment. For lifestyle-driven cases, some people can reduce or stop meds after major weight loss or dietary overhaul-but only under a doctor’s supervision and with regular monitoring.
Are plant-based diets better for cholesterol?
Yes, if they’re well-planned. Diets rich in vegetables, whole grains, legumes, nuts, and seeds consistently lower LDL. But not all plant-based diets are healthy-processed vegan foods, sugary snacks, and fried plant-based meats can still raise cholesterol. Focus on whole foods, not just avoiding animal products.
Final Thought: Your Cholesterol Isn’t Just a Number
It’s a reflection of your body’s long-term balance. Genetics play a role, but so do your meals, your movement, your sleep, your stress. You can’t change your genes-but you can change your habits. And that’s where real power lies.
Don’t wait for a crisis. Get tested. Talk to your doctor. Start small. One change today can mean years more with your family tomorrow.




John Mackaill
November 22, 2025 AT 02:56My dad had FH and didn't know until he had a heart attack at 48. They didn't even test him until he was 50. If we'd known earlier, he might still be here. Get tested if anyone in your family had early heart issues. Seriously.
Richard Wöhrl
November 22, 2025 AT 14:20Statins work-but here's the thing: not everyone responds the same. I had muscle pain at 10mg atorvastatin. Switched to ezetimibe + low-dose rosuvastatin, and my LDL dropped 48%. No pain. My doctor didn't even mention combo therapy at first. Ask for it.
Pramod Kumar
November 23, 2025 AT 13:01Bro, I used to think cholesterol was just about eggs and butter. Then I saw my dad's lipid panel-LDL 210, no obesity, no diabetes, just pure genetics. Turned out he had FH. We got tested. Me? LDL 198. Started on statin. Changed my life. Now I eat oats, nuts, lentils, and I'm not some vegan monk-just smarter. If you're Indian, you're at higher risk. Don't wait.
My aunt? She quit dairy, ate only rice and lentils, thought she was 'clean.' Her LDL stayed at 195. Turns out, refined carbs and ghee are silent killers. Food isn't just 'good' or 'bad'-it's about balance, not dogma.
And yes, inclisiran? I'm waiting for it to hit India. Twice-a-year shot? Sign me up. No more pills. No more forgetting. Just a quick jab and I'm done till next year. Life's too short for daily meds if you don't have to do them.
Brandy Walley
November 25, 2025 AT 08:50Statins cause diabetes and muscle damage. You're all being manipulated by Big Pharma. My cousin took them and got rhabdo. He's in a wheelchair. Don't be a sheep.
shreyas yashas
November 26, 2025 AT 21:48My mum had FH. We didn't know till she was 60. She had a stent. Now I'm 32, got tested, LDL 192. Doctor said 'just watch it.' I said 'nope.' Got genetic testing. Confirmed. Started on low-dose statin. Life's not about fear. It's about being proactive. You don't need to be perfect. Just consistent.
Also, non-fasting tests? Yes. I ate a samosa before mine. Results were spot on. No need to starve yourself before a simple blood draw. Doctors still tell people to fast like it's 2005.
Suresh Ramaiyan
November 28, 2025 AT 17:04Cholesterol isn't the enemy. It's the messenger. It shows us where our systems are out of balance-whether it's stress, sleep, inflammation, or just too many fried snacks from childhood. We treat the number, not the person. That's the problem. You can have perfect LDL and still have a heart attack if your arteries are inflamed from chronic stress or poor sleep. The real cure isn't a pill-it's a lifestyle that honors your body, not just one that chases numbers.
My friend dropped his LDL from 210 to 130 by quitting soda, walking 45 minutes daily, and sleeping 7 hours. No statin. He didn't go vegan. He just stopped pretending he was 'too busy' to care. Small things, done daily, add up. You don't need to overhaul your life. Just tweak it.
And if you're worried about statins? Talk to your doctor. Don't Google. Don't listen to Reddit gurus. Find someone who listens. That's the real medicine.
Katy Bell
November 29, 2025 AT 10:14I got my numbers checked after reading this. LDL was 203. I cried. Not because I'm scared-but because I realized I've been ignoring my body for years. I'm starting with walking. Just 20 minutes. No pressure. No guilt. Just me and my shoes.
Ragini Sharma
November 30, 2025 AT 22:14So basically if you're rich and white you get PCSK9 inhibitors but if you're brown and poor you get told to eat quinoa? Cool. Makes sense.
Linda Rosie
December 2, 2025 AT 08:32Genetic screening for familial hypercholesterolemia should be standardized in primary care. Early detection reduces long-term healthcare burden.
Vivian C Martinez
December 2, 2025 AT 15:00You got this. One small change today-swap soda for sparkling water, take the stairs, eat nuts instead of chips-those tiny wins add up. You're not failing if you slip. You're just learning. Keep going.
Ross Ruprecht
December 2, 2025 AT 20:23Why do we even care? People die of bad stuff all the time. Maybe cholesterol's just nature's way of thinning the herd.
Bryson Carroll
December 4, 2025 AT 14:52LDL is just a marketing tool invented by pharmaceutical companies to sell statins. Your body makes cholesterol because it needs it. Trying to lower it is like trying to lower your blood pressure by draining your veins. You're not fixing the problem-you're just suppressing a symptom.
Jennifer Shannon
December 4, 2025 AT 22:02I grew up in rural Alabama, where the word 'cholesterol' was only used in commercials for margarine. My grandpa ate bacon for breakfast, lunch, and dinner-and lived to 92. But he also walked three miles to church every Sunday, never owned a car, and never ate processed food. He didn't have a lipid panel. He just lived. We romanticize the past, but the truth is, most people back then didn't live long enough to get high cholesterol. Now we do-and we're not ready. We need to rebuild food systems, not just prescribe pills. The real epidemic isn't LDL-it's loneliness, food deserts, and the belief that health is a personal failure, not a societal one.
My sister, 34, got diagnosed with FH last year. She's on inclisiran now. She says it's the first time she's felt like her body isn't a ticking bomb. That matters. More than numbers. More than diets. It's about dignity.
And yes, eggs. I eat them. But I don't eat them with sausage and white toast. I eat them with spinach, mushrooms, and avocado. Context matters. Food isn't good or evil-it's a story. What's yours?
Suzan Wanjiru
December 6, 2025 AT 17:29Non-fasting tests are fine for screening but if your triglycerides are over 400 you still need to fast. Don't let anyone tell you otherwise. Also statins work better if you take them at night. Just saying.
Kezia Katherine Lewis
December 7, 2025 AT 22:10The clinical utility of polygenic risk scores in primary care settings remains underutilized despite robust evidence demonstrating incremental risk stratification beyond traditional lipid panels and familial history. Implementation science frameworks are urgently required to bridge the translational gap.