When a doctor prescribes a generic medication, most patients assume it’s just as safe and effective as the brand-name version. After all, the FDA says so. But behind the scenes, many clinicians are starting to ask harder questions - especially when a patient’s condition doesn’t improve, or worse, gets worse. The truth is, not all generic drugs are made the same. And where they’re made matters more than most people realize.
Where your generic drugs really come from
More than half of the active ingredients in generic medications today are produced in just two countries: India and China. The U.S. now makes only 14% of these critical components. The rest travel across oceans, through multiple factories, before ending up in a blister pack labeled with a familiar pharmacy brand. One company prints the label, but dozens may have touched the drug along the way - from chemical synthesis in a factory outside Hyderabad, to tablet pressing in a plant near Shanghai, to packaging in a warehouse in New Jersey. This global patchwork isn’t inherently bad. It’s cheap. And for a healthcare system under constant budget pressure, low cost is tempting. But when you’re cutting corners on manufacturing, quality can slip through the cracks. Older generics, especially, are the most vulnerable. As competition drives prices down, manufacturers have less money to invest in modern equipment or rigorous testing. Some are using decades-old machinery that can’t maintain consistent temperature, pressure, or purity levels - all critical for a drug to work properly.The hidden risk: adverse events tied to manufacturing location
A 2023 study from Ohio State University looked at over 1.2 million adverse event reports in the FDA’s database. They matched generic drugs made in the U.S. with identical versions made in India, controlling for dosage, patient age, and how often the drug was prescribed. What they found was startling: Indian-made generics were linked to 54% more severe adverse events - including hospitalizations, permanent disability, and even death - compared to their U.S.-made equivalents. This wasn’t random noise. The gap widened for older drugs that had been on the market for 10, 15, or even 20 years. These are the drugs that cost pennies per pill - the ones hospitals stock by the pallet. As price pressure mounts, some manufacturers cut costs in ways that aren’t visible on the label: skipping stability tests, using lower-grade excipients (inactive ingredients), or even substituting raw materials without disclosure. One cardiologist in Chicago told me about a patient on generic metoprolol who suddenly developed irregular heart rhythms. Switching to the brand version - same dose, same active ingredient - fixed it overnight. The patient had been stable for years. Nothing else changed. Just the generic. That’s not rare anymore. Clinicians are seeing it more often.Inspections that don’t inspect
The FDA claims its oversight is strong. And technically, it is - for U.S. facilities. The agency sends inspectors unannounced to domestic plants. They show up at 6 a.m. They check logs. They review data. They take samples. But for overseas factories? Inspections are scheduled weeks in advance. Manufacturers know exactly when they’re coming. They clean up. They fix the broken equipment. They hide the paperwork. It’s like a school inspection where the principal gets a heads-up. Professor Robert S. Gray, lead author of the Ohio State study, put it bluntly: “If you know an inspector is coming next Tuesday, you can make your plant look perfect. But that doesn’t mean it’s perfect on Monday - or Wednesday.” This isn’t just about honesty. It’s about capability. Many foreign plants still rely on manual processes. Temperature controls are inconsistent. Air filtration is outdated. Workers aren’t trained to the same standards as in U.S. facilities. And when something goes wrong - a batch of pills doesn’t dissolve properly, or a contaminant sneaks in - there’s no real accountability. The FDA can’t be everywhere. And when a drug fails, the blame often disappears into the supply chain.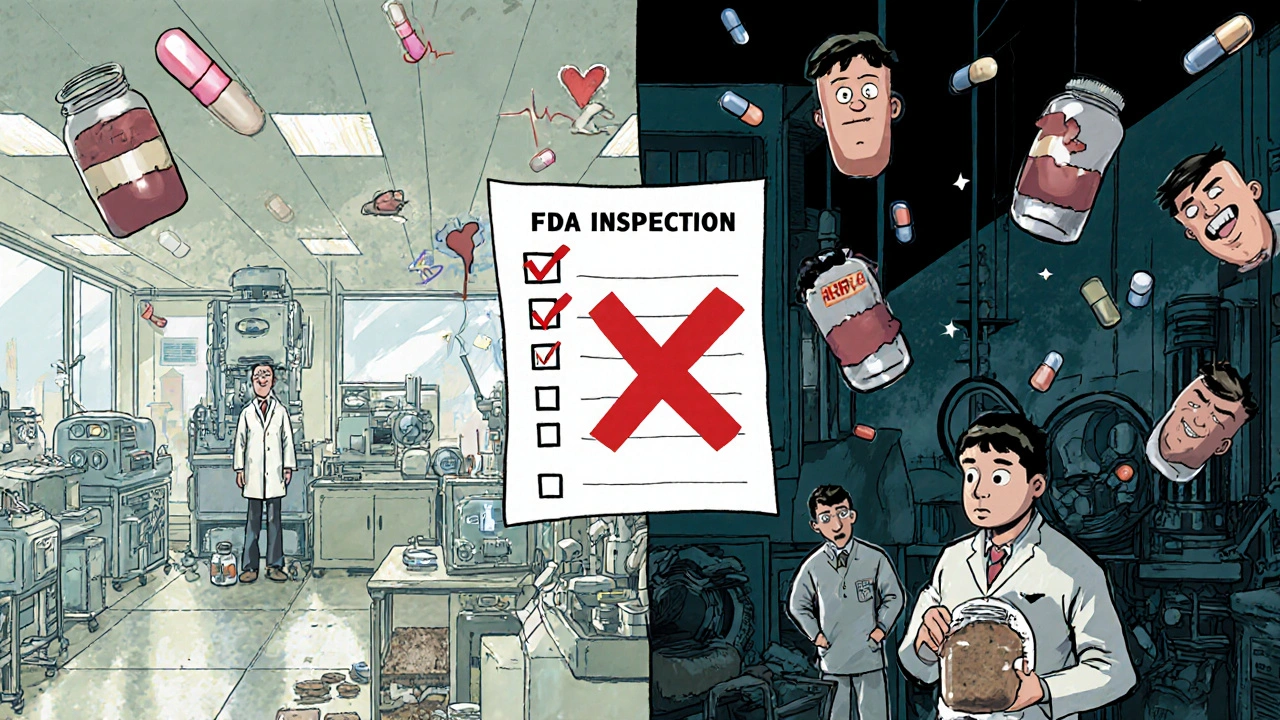
Why older generics are the most dangerous
Newer generics - those approved in the last five years - tend to be better made. Why? Because manufacturers are now using advanced manufacturing technologies (AMTs) like continuous production and real-time monitoring. These systems track every step of the process. They catch deviations before a single pill is made. Over 80% of drugs made with these technologies come from U.S. plants. But older generics? They’re stuck in the past. Think of them as analog drugs in a digital world. The original patent expired 20 years ago. No one’s investing in upgrades. The manufacturer doesn’t need to - because the price is so low, and no one’s asking questions. The FDA approves them based on bioequivalence: “Does it release the same amount of drug in the same time as the brand?” But bioequivalence doesn’t tell you if the drug dissolves too slowly in some patients. Or if it’s contaminated with trace metals. Or if the coating breaks down in humid conditions. That’s why drug shortages are rising - and why they’re concentrated in older generics. Duke-Margolis Center researchers call manufacturing quality the #1 cause of shortages. When a plant fails an inspection - or worse, has a quality incident - it’s not just one batch that’s recalled. It’s the entire supply. And if that plant is the only one making that specific generic? Patients go without.What clinicians are doing about it
Some doctors are starting to push back. Not by refusing generics altogether - that’s not practical. But by being more selective. A pharmacist in Minnesota started tracking which generic brands her patients responded to. She noticed that one brand of levothyroxine consistently caused heart palpitations. Another brand? Perfect. She started documenting this in patient charts. Now, when a new patient comes in with hypothyroidism, she asks: “Have you ever had issues with a generic thyroid med?” If yes, she prescribes the brand that worked before. Others are asking for transparency. They want to know where the drug was made - not just the label, but the actual manufacturing origin. Right now, that information isn’t required. But researchers at Ohio State are pushing the FDA to make it public. “If patients and providers could see that a drug was made in India versus the U.S., they could make informed choices,” says Gray. “It’s not about fear. It’s about fairness.” Some hospitals are even changing their formularies - the list of approved drugs. They’re removing the cheapest generic if it’s from a manufacturer with a history of FDA warning letters. They’re paying a little more for a version made in a facility with a clean inspection record.
Is there a solution?
There’s no single fix. But the pieces are there. Advanced manufacturing technologies can make drug production faster, cheaper, and far more reliable. The problem? The upfront cost is high. A single continuous manufacturing line can cost $50 million. Most generic manufacturers - especially those relying on low margins - can’t afford it. One solution? Incentivize domestic production. The University of Wisconsin School of Pharmacy argues that if more generic manufacturing happened in the U.S., we’d see fewer quality issues, fewer shortages, and a more resilient supply chain. That’s not just about patriotism. It’s about control. When you make drugs in your own country, you can inspect them. You can respond quickly. You can hold someone accountable. Another idea? Reward quality, not just price. Right now, the lowest bidder wins contracts for hospital drug supplies. What if instead, hospitals awarded contracts based on a manufacturer’s inspection history? Or their track record of recalls? Or their use of modern technology? That’s what Dr. Iyer from ASH Clinical News suggests: “Procurers can incentivize quality by ensuring that they only purchase from those who can demonstrate quality assurance.” The FDA is experimenting with this. They’ve launched pilot programs to fast-track inspections for manufacturers using advanced tech. But without policy changes, these efforts stay small.What patients should know
You don’t need to avoid generics. Most are safe. Most work fine. But if you’re on a generic drug that’s been on the market for a long time - especially if it’s for a chronic condition like heart disease, epilepsy, or thyroid disorder - pay attention. If your symptoms change suddenly, or if you’ve had side effects that didn’t happen before, ask your doctor: “Could this be the generic?” You can also ask your pharmacist: “Where was this made?” They may not always know - but they can check. And if they don’t, that’s a red flag too. The goal isn’t to scare people away from affordable medicine. It’s to make sure affordability doesn’t come at the cost of safety. Because when a drug fails, it’s not just a financial loss. It’s a missed dose of insulin. A seizure. A heart attack. A life changed.What’s next
The debate isn’t over. The FDA still says the system works. Industry groups say fears are overblown. But clinicians - the ones who see the real-world results - are speaking up. And they’re not backing down. The next five years will decide whether generics remain a pillar of affordable care - or become a hidden risk we can no longer ignore.Are generic drugs always safe?
Most generic drugs are safe and effective. But not all are made equally. Quality can vary based on where and how they’re manufactured. Older generics, especially those made overseas, have been linked to higher rates of serious side effects in recent studies. Always report unexpected side effects to your doctor.
Why are some generic drugs cheaper than others?
Price differences come from manufacturing costs. Drugs made in countries with lower labor and regulatory costs - like India or China - are cheaper. But lower cost doesn’t always mean lower quality. Some manufacturers cut corners on materials, testing, or equipment, which can affect how the drug performs in your body.
Can I tell where my generic drug was made?
Usually, no. The label only shows the brand name and the distributor. The actual manufacturing location is rarely listed. Some pharmacies may be able to check with their supplier, but this information isn’t required to be shared with patients. Advocates are pushing for transparency so consumers can make informed choices.
Should I avoid generics made in India or China?
Not necessarily. Many high-quality generics come from these countries. But if you’re on a long-term medication - especially one with a narrow therapeutic window like warfarin, levothyroxine, or seizure drugs - and you notice new side effects, ask your doctor about switching to a different generic brand or the brand-name version. Don’t assume all generics are identical.
What’s being done to fix this problem?
Researchers and clinicians are calling for more transparency in manufacturing origins, unannounced global inspections by the FDA, and incentives for manufacturers to use advanced production technologies. Some hospitals are already switching to generics from suppliers with better inspection records. The FDA is testing new programs, but major policy changes are still slow to come.






Emily Entwistle
November 18, 2025 AT 06:36This is wild, but honestly? I switched my thyroid med last year after my heart started racing. Same dose, same 'generic'-but different maker. Boom. Instant calm. 🤯 Don’t assume they’re all the same. Ask your pharmacist where it’s from. They can check! 😊
Hannah Blower
November 19, 2025 AT 22:12Of course the FDA’s oversight is a joke. You think they’re going to risk the $200B pharmaceutical-industrial complex? The real scandal isn’t that generics are dangerous-it’s that we’ve outsourced our health to a supply chain where quality control is an afterthought, and profit is the only KPI. We’re not patients. We’re data points in a Bloomberg terminal. And now we’re surprised when the algorithm crashes?
It’s not about India or China. It’s about capitalism. When you commodify medicine, you commodify human lives. And guess what? The people who pay the price aren’t the ones voting on the FDA budget.
Gregory Gonzalez
November 21, 2025 AT 21:13Wow. A 54% increase in adverse events? How shocking. I bet the next study will find that breathing air made in China causes 78% more coughing. At this rate, we’ll soon need to ban all imported oxygen.
But seriously-this is why I love American journalism. Turning a complex, nuanced issue into a ‘Made in China = Death’ headline. The real crisis? Our inability to handle gray areas. Maybe the problem isn’t the pills… it’s our fear of complexity.
Ronald Stenger
November 22, 2025 AT 01:40Let’s cut the crap. We let China and India make our medicine because we’re too lazy to make it ourselves. Now we’re shocked when the medicine breaks? Wake up. We gave up our manufacturing base for cheap socks and phone chargers. Now we’re paying for it with lives. And the worst part? The same people who cried ‘offshoring bad!’ for factories are silent when it’s pills. Hypocrisy is the American pastime.
Stop whining. Start demanding domestic production. If you want safe meds, pay for them. Or shut up when your grandma gets sick because you wanted a $3 refill.
Samkelo Bodwana
November 23, 2025 AT 05:22As someone from South Africa, where we rely heavily on Indian-made generics for HIV and TB meds, I’ve seen both sides. Yes, there are bad batches. Yes, some plants cut corners. But I’ve also seen life-saving drugs made in Hyderabad that kept my cousin alive for 12 years when the brand version was unaffordable. The issue isn’t geography-it’s regulation and oversight. We need global standards, not nationalist fear. India has world-class pharma companies-some even supply the WHO. Blaming a country ignores the real problem: profit-driven systems that prioritize cost over care, everywhere.
Instead of fear, let’s demand transparency. Let’s push for independent audits, not just FDA visits that are scheduled like dentist appointments. And let’s fund the development of quality control systems that work globally, not just in the U.S. We’re all in this together.
Duncan Prowel
November 23, 2025 AT 13:34While the data presented is compelling, one must consider potential confounding variables: patient adherence, comorbidities, pharmacokinetic variability, and the possibility of reporting bias in the FDA’s voluntary adverse event system. The assertion that Indian-made generics are inherently more dangerous requires further stratification by manufacturer, batch number, and specific excipient profiles. Without such granularity, the correlation may be misleading. That said, the systemic failure of post-market surveillance remains a legitimate concern.
Bruce Bain
November 23, 2025 AT 23:14I get it. You’re scared. I’m scared too. But here’s the thing: I’ve been on generic metoprolol for 8 years. My blood pressure’s fine. My heart’s fine. My wallet’s fine. Not every generic is bad. Most are fine. But if your body acts weird? Switch. Talk to your doc. Don’t panic. Just pay attention. That’s all.
Jonathan Gabriel
November 25, 2025 AT 21:25So… the FDA inspects U.S. plants unannounced but gives foreign plants a heads-up? That’s not negligence. That’s a feature. They know the system’s broken. They’re just too busy playing politics to fix it. And now we’re supposed to trust a 20-year-old generic made in a factory with a 1987 tablet press? Please. The real conspiracy? That we’re told this is ‘safe’ while the same companies that make these pills also fund the FDA’s budget. It’s not a glitch. It’s the design.
And don’t get me started on ‘bioequivalence.’ That’s like saying two cars are the same because they both have four wheels and a gas pedal. One could be a Tesla. The other? A rusted Yugo with a broken fuel pump. But hey, the odometer says ‘same miles per gallon.’
Don Angel
November 25, 2025 AT 23:33Look. I’m not anti-generic. I’m pro-safety. If my doctor prescribes a generic, I’m fine with it-unless I’ve had a bad reaction before. Then I ask for the brand. Or a different maker. Simple. I don’t need a lecture. I just want to know: ‘Is this the same pill that worked last time?’ If the answer is ‘we don’t know,’ that’s a problem. Let’s fix that.
benedict nwokedi
November 27, 2025 AT 04:11They’re not just making bad pills-they’re making them on purpose. The deep state wants us dependent. Weak. Sick. So they can control us with meds. Why else would they let a country with zero human rights standards make 60% of our life-saving drugs? It’s not about money. It’s about population control. And now they’re pushing ‘transparency’ to distract us from the real agenda: total pharmaceutical domination. Check the patents. Check the ownership. The same CEOs who own Pfizer own the Indian factories. It’s all connected.
deepak kumar
November 28, 2025 AT 10:49As someone from India, I want to say this: We make 40% of the world’s generics. And yes, some factories cut corners. But many of us are proud of our quality. I’ve visited plants in Hyderabad that are cleaner than some U.S. labs. The problem isn’t India-it’s the race to the bottom. When a U.S. hospital buys the cheapest bid, they’re not just choosing a price-they’re choosing a risk. We can fix this by rewarding the good manufacturers, not punishing the whole country. Many of us want to do better. We just need fair prices to do it.
Dave Pritchard
November 29, 2025 AT 06:40Hey, if you’re on a long-term med and something feels off-don’t ignore it. Talk to your doctor. Ask for the maker. Try a different brand. You’re not being paranoid-you’re being smart. And if your pharmacist doesn’t know where it’s from? That’s not their fault. It’s the system’s. But you can still ask. Keep asking. Your health matters more than the price tag.
kim pu
November 30, 2025 AT 00:20OMG I KNEW IT. The FDA is just a puppet for Big Pharma and the globalist cabal. They let China make our meds because they’re trying to depopulate us with substandard pills that cause ‘random’ heart attacks. I’ve been tracking my pills since 2020. I only take the ones with the ‘USP’ stamp-because I know the real ones are made in secret Swiss bunkers. The rest? Poison. 🧪💀
malik recoba
December 1, 2025 AT 19:00just wanna say thank you for writing this. i’ve been on generic warfarin for years and my INR kept spiking. i switched brands last month and now i’m stable. i didn’t know why. now i do. i’m gonna tell my mom to ask her pharmacist too. it’s scary but i’m glad someone’s talking about it. thank you.