
Bipolar Antidepressant Risk Calculator
Risk Assessment Tool
Estimate your personal risk of mood switching when taking antidepressants based on bipolar disorder type and other factors.
Your risk of mood destabilization is calculated when you click "Calculate Risk".
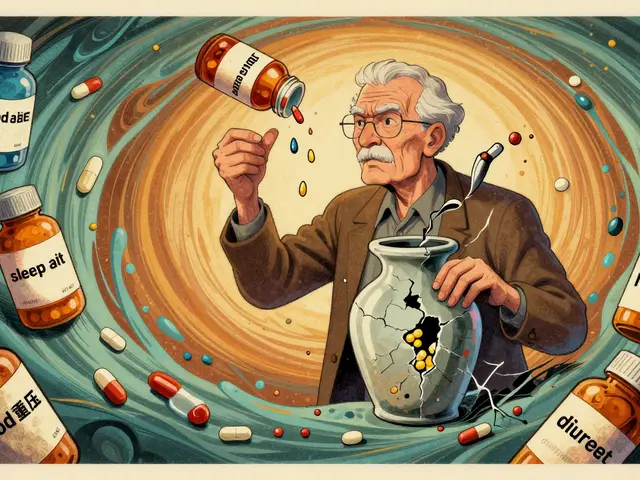
When someone with bipolar disorder feels deep, crushing depression, it’s tempting to reach for an antidepressant. After all, they work for unipolar depression. But in bipolar disorder, that simple solution can backfire-sometimes dramatically. What looks like improvement can quickly turn into mania, rapid cycling, or a mixed state where sadness and agitation crash together. This isn’t rare. It’s well-documented. And yet, antidepressants are still prescribed far too often.
Why Antidepressants Are Risky in Bipolar Disorder
Antidepressants were never designed for bipolar disorder. They were made for unipolar depression-where there’s only one mood pole: low. Bipolar disorder has two: low and high. Introducing a drug that lifts mood in someone whose brain already swings between extremes can tip the balance. Instead of easing depression, it can trigger a switch into mania or hypomania. Studies show that about 12% of people with bipolar disorder who take antidepressants experience a polarity switch-meaning their depression flips into mania. That number jumps to 31% in real-world, retrospective data. For comparison, the natural switch rate with mood stabilizers alone is around 10.7%. So antidepressants don’t just add benefit-they add risk. The risk isn’t the same for everyone. People with Bipolar I, a history of prior antidepressant-induced mania, rapid cycling, or mixed features during depression are at highest risk. In fact, if you’ve had one episode triggered by an antidepressant before, your chance of it happening again is more than three times higher.Not All Antidepressants Are Equal
Some antidepressants are riskier than others. Tricyclics like amitriptyline carry the highest switch risk-up to 25%. SNRIs like venlafaxine aren’t much better. But SSRIs like sertraline or escitalopram? They’re lower, around 8-10%. Bupropion (Wellbutrin) is often preferred because it doesn’t strongly affect serotonin, which may reduce the chance of triggering mania. Still, even SSRIs can cause problems. One patient in Leeds told me their doctor prescribed sertraline for a depressive episode. Within two weeks, they were sleeping only two hours a night, spending money recklessly, and convinced they were on a special mission. Hospitalized. That’s not an outlier. It’s a known pattern. The bottom line: no antidepressant is safe in bipolar disorder without a mood stabilizer or atypical antipsychotic in place. Even then, the benefit is small.The Numbers Don’t Add Up
Let’s look at the math. For unipolar depression, antidepressants work well. You need to treat about 6-8 people to see one respond. In bipolar depression? You need to treat nearly 30 people to get one meaningful response. That’s a huge difference. Meanwhile, the number needed to harm-how many people you have to treat before one has a switch-is about 200. Sounds low risk? Not when you consider how many people are on these drugs. With an estimated 50-80% of bipolar patients in the U.S. being prescribed antidepressants, that’s tens of thousands of people at risk every year. And here’s the kicker: antidepressants don’t even help prevent relapse. In fact, long-term use (over 24 weeks) increases the chance of future depressive episodes by 37%. They may help in the short term, but over time, they can make the illness worse.
What Works Better
The FDA has approved four medications specifically for bipolar depression-and none are traditional antidepressants:- Quetiapine (Seroquel): 50-60% response rate, less than 5% switch risk
- Lurasidone (Latuda): 50% response rate, only 2.5% switch risk
- Cariprazine (Vraylar): 48% response rate, 4.5% switch risk
- Olanzapine-fluoxetine (Symbyax): 50% response rate, 5-7% switch risk
Who Should Even Consider Antidepressants?
The International Society for Bipolar Disorders (ISBD) 2022 guidelines are clear: antidepressants should be avoided as monotherapy. They should only be used as a short-term add-on in severe, treatment-resistant cases-after at least two FDA-approved treatments have failed. Even then, they’re not for everyone. Avoid them if you have:- Bipolar I disorder
- A history of antidepressant-induced mania
- Four or more mood episodes per year (rapid cycling)
- Mixed features (depression with agitation, irritability, racing thoughts)
Monitoring and What to Watch For
If an antidepressant is used, weekly check-ins for the first month are non-negotiable. Look for early signs of mania:- Needing less sleep but feeling energized
- Racing thoughts or pressured speech
- Impulsive spending, risky sex, or reckless decisions
- Unusual irritability or anger
- Grandiose ideas (“I can start a company,” “I’m destined for greatness”)
Why Do Doctors Still Prescribe Them?
If the risks are so clear, why are antidepressants still used in 80% of community clinics? Three reasons:- Diagnosis errors: Nearly 40% of bipolar disorder cases are misdiagnosed as unipolar depression at first. If you think someone has regular depression, antidepressants seem logical.
- Pressure from patients: People in deep depression beg for something that works fast. Mood stabilizers take weeks. Antidepressants can show results in 2-4 weeks.
- Clinical inertia: It’s easier to keep prescribing what’s familiar than to switch to a complex regimen with multiple meds and close monitoring.
What Patients Need to Know
If you have bipolar disorder and are on an antidepressant:- Ask your doctor: “Is this FDA-approved for bipolar depression?”
- Ask: “What’s my risk of switching?”
- Ask: “Am I on a mood stabilizer or antipsychotic too?”
- Ask: “How long will I be on this?”
The Bigger Picture
We’re in a transition. For decades, bipolar depression was treated like unipolar depression. That was a mistake. Now, the science is catching up. Guidelines are clearer. Alternatives are better. And the risks of antidepressants are no longer debated-they’re proven. The real challenge isn’t finding a new drug. It’s changing how we think. Bipolar disorder isn’t depression with mood swings. It’s a distinct illness with its own rules. Treating it like unipolar depression doesn’t just miss the mark-it can make things worse. The goal isn’t just to lift mood. It’s to stabilize it. And that’s not something an antidepressant can do alone.Can antidepressants cause mania in bipolar disorder?
Yes. Antidepressants can trigger mania or hypomania in people with bipolar disorder, especially if used without a mood stabilizer. Studies show about 12% of patients experience a polarity switch, with higher rates in those with Bipolar I, rapid cycling, or prior switch history.
Are SSRIs safer than other antidepressants for bipolar depression?
SSRIs carry a lower risk of mood switching (8-10%) compared to tricyclics (15-25%) or SNRIs. But they’re not safe. Even SSRIs can trigger mania, especially without a mood stabilizer. Bupropion is often preferred because it has less effect on serotonin, but it still carries risk.
What are the FDA-approved treatments for bipolar depression?
The FDA has approved four medications specifically for bipolar depression: quetiapine (Seroquel), lurasidone (Latuda), cariprazine (Vraylar), and the combination of olanzapine and fluoxetine (Symbyax). These have better safety profiles than antidepressants, with switch risks under 5% and response rates of 48-60%.
How long should antidepressants be used in bipolar disorder?
If used at all, antidepressants should be limited to 8-12 weeks as a short-term add-on for severe, treatment-resistant cases. Long-term use increases the risk of rapid cycling and more frequent episodes. The ISBD recommends discontinuing them regardless of response after this period.
Can antidepressants make bipolar disorder worse over time?
Yes. Long-term use (over 24 weeks) is linked to a 37% higher risk of future depressive episodes and may promote rapid cycling. Antidepressants don’t stabilize mood-they can destabilize it. This is why professional guidelines now recommend avoiding them unless absolutely necessary.
What should I do if I think an antidepressant triggered my mania?
Stop taking the medication immediately and contact your psychiatrist. Do not wait or try to adjust the dose. Document the timeline of symptoms and bring it to your next appointment. Never take that antidepressant again. Your history of a switch is a strong predictor of future episodes if you reuse it.


Billy Schimmel
December 5, 2025 AT 07:20So you're telling me we've been treating a complex mood disorder like a cold with antibiotics for decades? And now we're surprised people keep getting sicker?
pallavi khushwani
December 7, 2025 AT 01:23I've seen this play out in my family. My cousin was on sertraline for 'depression'-turned into a sleepless, credit-card-maxing mess in 11 days. No one connected the dots until she was in the ER. It's terrifying how common this is-and how rarely doctors warn us.
Why do we keep pretending bipolar is just depression with mood swings? It's not. It's a different disease. We need to stop treating symptoms and start treating the whole system.
Dan Cole
December 7, 2025 AT 15:40Let’s be precise: the 12% switch rate cited is from RCTs-highly controlled, exclusionary populations. Real-world data (as you rightly note) shows 31%. That’s not a statistical anomaly. That’s a clinical catastrophe.
And yet, psychiatry still clings to the serotonin hypothesis like a religious dogma. We’ve known since the 1990s that bipolar isn’t a serotonin deficiency-it’s a dysregulation of circadian, glutamatergic, and dopaminergic systems. SSRIs don’t fix that. They destabilize it.
Also, the fact that we still use tricyclics in 2024 is criminal. They’re 1950s tech with 2020s side effects. Why are we still prescribing them? Because medical education is a fossil.
Shayne Smith
December 8, 2025 AT 08:02My therapist said the same thing. She told me to stop asking for antidepressants and start asking for 'mood stabilizers.' I didn’t even know those were a thing until I read this. I thought bipolar meant you were just moody.
Now I’m on lurasidone. I sleep. I don’t spend my rent money on Amazon. I don’t think I’m Elon Musk’s secret daughter.
Thank you for writing this.
Kay Jolie
December 9, 2025 AT 02:44As someone who’s been in the trenches of affective neuroscience for 14 years, I can say with clinical certainty: the paradigm shift is here. The old model of 'depression = low serotonin' is not just outdated-it’s dangerously reductive.
What’s fascinating is how the FDA-approved agents-quetiapine, lurasidone, cariprazine-all modulate D3 receptors. That’s the real key. Not serotonin. Not norepinephrine. Dopamine D3. And yet, we still treat bipolar depression with drugs that ignore this entirely.
It’s not negligence. It’s institutional inertia. Pharma doesn’t profit from repurposing antipsychotics. They profit from selling SSRIs forever.
Max Manoles
December 10, 2025 AT 11:45One thing nobody talks about: the placebo effect in bipolar depression trials is absurdly high. Up to 40% in some studies. That means the 'efficacy' of antidepressants is often just noise.
Meanwhile, the real-world harm-rapid cycling, mixed episodes, treatment resistance-isn’t measured in RCTs. It’s measured in ER visits, job losses, divorces, and suicide attempts.
We need longitudinal data. We need real-world evidence. And we need to stop pretending that 'it worked for me' is a valid clinical argument when the cost is destabilizing an entire neurobiological system.
Katie O'Connell
December 11, 2025 AT 23:25While the data presented is compelling, one must consider the epistemological limitations of retrospective studies. The 31% switch rate is derived from self-reported, non-blinded, uncontrolled cohorts-methodologically unsound. Furthermore, the FDA-approved agents carry metabolic burdens that may be more detrimental long-term than transient manic switches.
One cannot simply dismiss decades of clinical experience with SSRIs on the basis of epidemiological trends. Individualized medicine requires nuance, not dogma.
Mansi Bansal
December 12, 2025 AT 04:50It is imperative that we recognize the profound ethical implications of this clinical misalignment. The continued prescription of antidepressants in bipolar populations constitutes a violation of the principle of non-maleficence.
Furthermore, the cultural normalization of pharmacological quick-fixes in Western psychiatry reflects a deeper societal pathology: the commodification of mental health, wherein emotional suffering is reduced to a biochemical imbalance amenable to commercial solutions.
One must question the hegemony of the DSM paradigm, which pathologizes natural human variation under the guise of scientific objectivity.
Jackie Petersen
December 14, 2025 AT 02:00Wait. So you're saying the government and Big Pharma are lying to us? Again? Just like with opioids? Just like with antidepressants for kids? Just like with vaccines? I knew it. I KNEW IT.
They don't want us to heal. They want us to stay sick and keep buying pills. This is a psyop. They're using bipolar people as guinea pigs to sell more drugs. Who's behind this? Who funded this study? Who owns the journal?
Mayur Panchamia
December 14, 2025 AT 10:13India has been treating bipolar disorder with antidepressants for 30 years-and we’re still here. Still breathing. Still working. Still loving.
What do you know about Indian patients? We don’t have access to lurasidone. We don’t have psychiatrists in every town. We have one pill. We take it. We survive.
Don’t lecture us about 'risk' when we’re fighting for basic care. Your guidelines are for rich countries. We need what works now-not what’s perfect in a Harvard lab.
Ashish Vazirani
December 15, 2025 AT 03:21OH MY GOD. YES. YES. YES.
I was prescribed fluoxetine in 2018. Two weeks later, I was in a hotel in Goa, convinced I was the reincarnation of Shiva, selling my laptop to buy crystals, and screaming at strangers that I was going to 'fix the economy.'
They called it 'manic episode.' I call it 'the day I realized my doctor didn’t know what the fuck he was doing.'
Now I’m on quetiapine. I sleep. I pay my bills. I don’t think I’m a god. I’m just… me.
Thank you. I’ve been waiting 6 years for someone to say this out loud.
Kumar Shubhranshu
December 15, 2025 AT 07:01Stop prescribing SSRIs for bipolar. Done.
Clare Fox
December 16, 2025 AT 18:44i’ve been on an antidepressant for 3 years. i thought it was helping. turns out i was just… more manic, but quieter. like, i didn’t scream at people, i just bought 17 pairs of shoes and wrote 400 pages of a novel no one asked for.
my doctor said ‘it’s working.’
turns out, ‘working’ means ‘making you a little bit unhinged but polite.’
im done.
Akash Takyar
December 18, 2025 AT 07:54As a mental health advocate in rural India, I have witnessed the devastating consequences of misdiagnosis and inappropriate medication. Many families cannot afford specialist care. They rely on general practitioners who prescribe antidepressants because they are cheap and accessible.
We need training programs for primary care doctors. We need telepsychiatry. We need awareness campaigns in local languages. The science is clear-but it must reach the villages, not just the cities.
Let us not condemn the doctors; let us equip them.
Arjun Deva
December 20, 2025 AT 05:15Who is funding this? Who wrote this? Is this a covert attempt to push antipsychotics? Because I know the truth: antidepressants are being phased out because the pharmaceutical companies are losing money on them. They want to sell you expensive, patent-protected antipsychotics instead.
And don’t even get me started on esketamine. That’s a gateway drug for corporate psychiatry. They’re turning emotional pain into a $1,000 nasal spray.
They don’t want you to heal. They want you to be dependent.
Annie Gardiner
December 20, 2025 AT 16:55Wow. So now we’re supposed to believe that antidepressants are evil because they sometimes cause mania? What about the people who get relief? What about the ones who don’t switch? Are their experiences invalid because they don’t fit your narrative?
Also, why is it that every time someone suggests a new treatment, it’s always ‘this is the only way’? You sound like a cult leader with a PubMed account.
Andrew Frazier
December 20, 2025 AT 19:46Let’s be real-this is just woke psychiatry. You want to ban antidepressants because they’re ‘Western’? We’re talking about real people here. People who are suffering. People who need help now.
Meanwhile, in the real world, people are dying from untreated depression. You want to take away their only tool because some study says ‘maybe’ it could trigger mania?
That’s not medicine. That’s moral panic.
Karen Mitchell
December 21, 2025 AT 15:50It is morally indefensible to subject vulnerable individuals to pharmacological interventions with known destabilizing potential, particularly when safer alternatives exist. The persistence of this practice reflects a systemic failure of medical ethics, where profit and convenience override the sanctity of human neurobiology.
Furthermore, the normalization of such practices within clinical training institutions constitutes a profound corruption of the healer’s oath.
Kay Jolie
December 21, 2025 AT 21:02Response to @5646: The issue isn’t about ‘narratives.’ It’s about risk-benefit ratios. You can’t dismiss 30% of patients experiencing mania as ‘anecdotes.’ That’s not skepticism-that’s denial.
And yes, I know people get relief. But if you’re trading 10 weeks of stability for 10 years of rapid cycling, is that really relief? Or just delayed harm?
And if you’re telling me ‘I’m one of the 70% who didn’t switch,’ that’s great. But you’re not the only patient in the room. The data isn’t about you. It’s about the population.
Max Manoles
December 23, 2025 AT 11:48Response to @5648: You’re framing this as ‘taking away tools.’ But we’re not taking anything away. We’re offering better tools.
Quetiapine isn’t ‘woke.’ It’s a drug with a 5% switch risk and a 60% response rate. That’s not ideology. That’s pharmacology.
And if you think people are dying from ‘untreated depression’ because we’re not prescribing SSRIs-you’re ignoring the fact that SSRIs are often prescribed to people who don’t have unipolar depression at all.
It’s not about denying care. It’s about giving the right care.