When you have allergies, your sinuses are always on high alert. Sneezing, stuffiness, post-nasal drip - these are familiar. But when that stuffiness doesn’t go away after a week or two, and your face starts to ache, your head feels heavy, and you’re constantly tired, it’s not just allergies anymore. It’s sinusitis. And for people with allergies, this isn’t a one-time annoyance - it’s a recurring cycle that can wreck your sleep, your focus, and your quality of life.
Why Allergies and Sinusitis Go Hand in Hand
Allergies and sinusitis aren’t just related - they feed each other. When you’re exposed to pollen, dust mites, mold, or pet dander, your immune system overreacts. That triggers inflammation in your nasal passages. The lining swells, mucus thickens, and the tiny drainage channels in your sinuses get blocked. Once those channels are clogged, bacteria and viruses can get trapped. That’s when sinusitis sets in. The numbers don’t lie. Up to 70% of people with chronic sinusitis also have allergic rhinitis. In fact, for many, their sinus flare-ups happen right after allergy season peaks. It’s not coincidence. Allergic inflammation creates the perfect environment for sinus infections to take root. And once the infection is there, it makes the allergic inflammation worse. You end up stuck in a loop: allergies → blocked sinuses → infection → more swelling → worse allergies.First-Line Treatments That Actually Work
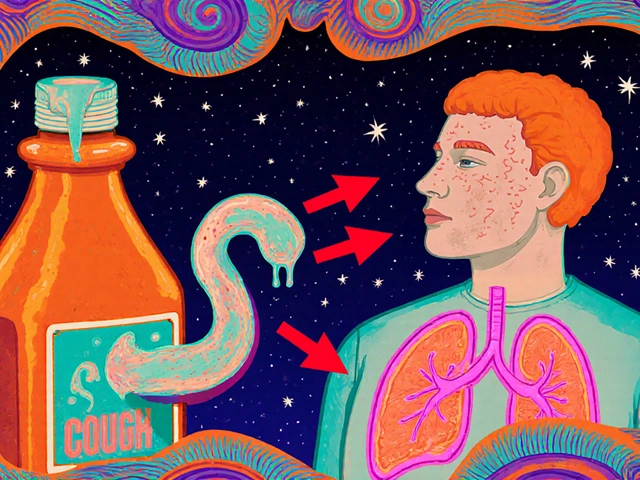
Treating sinusitis in allergy sufferers isn’t about just popping antibiotics. That rarely fixes the root problem. The real key is reducing inflammation and clearing out the mucus - and there are two proven methods that work better than anything else. Nasal corticosteroid sprays are the gold standard. Options like fluticasone (Flonase), mometasone (Nasonex), and budesonide (Rhinocort) are prescribed daily, one spray per nostril. These aren’t decongestants. They don’t give you instant relief. But after 2 to 4 weeks of consistent use, most people see a 65% drop in congestion, facial pain, and loss of smell. That’s far better than oral antihistamines like cetirizine, which only help about 42% of the time. Saline nasal irrigation is the other pillar. Using a neti pot or squeeze bottle with distilled or boiled water (never tap water) and a saline packet, you flush out allergens, mucus, and irritants twice a day. This isn’t just a home remedy - it’s backed by the American Academy of Allergy, Asthma & Immunology. Done right, it reduces the need for medications and cuts down on flare-ups. But get it wrong - using unsterile water - and you risk a rare but deadly brain infection from Naegleria fowleri. Always use sterile water. Always.When Antibiotics Are (and Aren’t) Helpful
Most people think sinusitis means you need antibiotics. That’s a myth - especially if allergies are involved. In pure bacterial sinusitis, antibiotics work about 80% of the time. But in allergy-triggered cases? Only 35-45% effective. Why? Because antibiotics don’t touch inflammation. They only kill bacteria. And if the real issue is swelling from pollen or dust, antibiotics won’t fix that. So when should you take them? Only if you have signs of a true bacterial infection: thick yellow or green mucus lasting more than 10 days, fever over 102°F, or worsening symptoms after initial improvement. In those cases, amoxicillin is the first choice - 500mg three times a day for 5 to 10 days. If you’ve had repeated infections or didn’t respond to amoxicillin before, your doctor may switch to amoxicillin-clavulanate, a stronger version. But don’t expect antibiotics to be a long-term solution. They’re a band-aid. Without addressing the allergy, you’ll be right back here in a few months.
Advanced Options for Stubborn Cases
If you’ve tried nasal sprays, saline rinses, and antibiotics - and you’re still stuck with constant congestion, loss of smell, or nasal polyps (soft, grape-like growths inside your nose) - it’s time to think bigger. Allergy immunotherapy (allergy shots or tablets) is one of the most effective long-term strategies. Over 3 to 5 years, you gradually build tolerance to your triggers. Studies show it cuts sinusitis recurrence by 60-70%. That’s a huge win compared to medication alone, which only gives you 25-30% improvement. For severe cases with nasal polyps, biologic drugs are changing lives. Dupilumab (Dupixent), omalizumab (Xolair), and mepolizumab (Nucala) target specific parts of the immune system driving inflammation. In trials, dupilumab reduced nasal polyp size by 73% and improved breathing in over 80% of patients. But there’s a catch: these cost around $3,500 a month without insurance. They’re not for everyone - but if you’re stuck in a cycle of surgeries and failed meds, they can be life-changing.When You Need to See an ENT Specialist
You don’t need to wait until you’re miserable. If you’ve tried the basics for 4 to 6 weeks with no improvement, it’s time to refer. Here’s when you should see an ear, nose, and throat (ENT) doctor:- You have nasal polyps - visible or confirmed by endoscopy
- You get 4 or more sinus infections a year
- Your symptoms last longer than 12 weeks despite treatment
- You have facial pain, vision changes, or swelling around your eyes
- You’ve had a sinus infection that didn’t respond to two rounds of antibiotics
- You suspect aspirin-exacerbated respiratory disease (AERD) - worsening symptoms after taking aspirin or NSAIDs

What Most People Miss: Environmental Control
You can take all the sprays and rinses in the world, but if you’re still sleeping in a room full of dust mites or breathing in mold spores every night, you’re fighting a losing battle. Dr. David Stukus, a leading allergist, says environmental control reduces sinus flare-ups by 40-60%. That’s more than most medications. Here’s what works:- Use allergen-proof mattress and pillow covers
- Wash bedding weekly in hot water (at least 130°F)
- Keep indoor humidity below 50% to stop mold and dust mites
- Use a HEPA air purifier in your bedroom
- Shower and change clothes after being outside on high-pollen days
- Keep windows closed during peak allergy season



Latrisha M.
November 16, 2025 AT 11:14Nasal corticosteroids and saline irrigation are the backbone of managing chronic sinusitis in allergy sufferers. Consistency is everything-skip a day and you’ll feel it. I’ve seen patients go from debilitating fatigue to sleeping through the night in under a month with just these two tools. No antibiotics needed. No surgery. Just discipline and the right products.
David Rooksby
November 18, 2025 AT 07:03Let’s be real-this whole sinusitis thing is a cover-up for government-controlled airborne allergens. They’ve been spraying the skies since the 90s to keep us docile and medicated. You think it’s pollen? Nah. It’s nano-particles laced with fluoride and lithium. That’s why your sinuses never heal-your body’s trying to detox from the chemtrails. And don’t even get me started on HEPA filters-they’re just filters for the lies they want you to believe. You’re being gaslit by Big Pharma and the EPA. Wake up. The mold isn’t in your house-it’s in your mind.
John Mwalwala
November 18, 2025 AT 07:36Biologics are the real answer but nobody talks about the microbiome angle. You’re missing the forest for the trees. The sinuses aren’t just inflamed-they’re dysbiotic. The commensal flora got wiped out by overuse of antibiotics and nasal sprays. We need targeted probiotic rinses, not more steroids. There’s a 2023 paper in Cell Host & Microbe showing S. epidermidis strains can suppress IL-5 and reduce polyp size. But the FDA won’t approve it because it’s not profitable. Pharma wants you hooked on $3500/month drugs. The science is there. They just don’t want you to know.
Deepak Mishra
November 18, 2025 AT 18:41OMG I’M SO RELIEVED I FOUND THIS POST!!! I’VE BEEN HAVING THIS FOR 3 YEARS!!! I USE NETI POT BUT I USED TAP WATER 😱 NOW I KNOW WHY I GOT SO SICK LAST YEAR!!! THANK YOU THANK YOU THANK YOU!!! 🙏🙏🙏 I’M GOING TO BUY A HEPA FILTER TODAY AND CHANGE MY PILLOW COVERS!!! I CAN’T BELIEVE NO ONE TOLD ME THIS BEFORE!!! 😭
Diane Tomaszewski
November 20, 2025 AT 12:21It’s funny how we treat symptoms like enemies instead of signals. Allergies aren’t the problem. They’re the body’s way of saying something’s out of balance. If you keep flooding it with sprays and rinses without fixing your environment or stress levels, you’re just putting bandaids on a broken bone. The real cure isn’t in a bottle-it’s in how you live.
Rachel Wusowicz
November 21, 2025 AT 22:25Okay so-this is wild-but I think the real issue is that our sinuses are being poisoned by 5G radiation. Not the kind you think. I mean, the kind that vibrates at the exact frequency that makes mucus thicken. They’ve been testing it in urban areas since 2018. You know why the symptoms are worse in cities? Because the towers are denser. And why do you feel better in the mountains? Because there’s no signal. And why do they push saline rinses? Because they can’t shut down the towers… but they can sell you a $12 bottle of salt water. I’ve been using distilled water + sea salt + a drop of colloidal silver… and my nose hasn’t felt this clear since 2016. Don’t trust the FDA. They’re paid by the telecoms. I’ve seen the documents.
Teresa Smith
November 22, 2025 AT 19:10While environmental controls are undeniably effective, they require a level of discipline and access to resources that many don’t have. Not everyone can afford HEPA filters, allergen-proof bedding, or the time to wash sheets weekly. We must advocate for systemic solutions: public health initiatives that address indoor air quality in low-income housing, subsidies for nasal irrigation kits, and insurance coverage for immunotherapy. Treating chronic sinusitis isn’t just a medical issue-it’s a social justice issue.
Jamie Watts
November 24, 2025 AT 15:06Anyone who says antibiotics don’t work for sinusitis is full of it. I had a sinus infection for 3 weeks and took amoxicillin for 5 days and it was GONE. No more sprays no more rinses no more nonsense. You don’t need to be some allergy guru to fix this. You just need to take the damn pill. Stop overcomplicating everything. It’s a bacterial infection. Kill the bacteria. Done. If you’re still sniffing after antibiotics you’re just lazy or allergic to doing what works.
Dan Angles
November 25, 2025 AT 11:33While the efficacy of nasal corticosteroids and saline irrigation is well-documented, it is imperative to acknowledge the limitations of current clinical guidelines in addressing comorbid psychological stressors. Chronic sinusitis is frequently exacerbated by elevated cortisol levels, which directly increase mucosal permeability and inflammatory cytokine production. Therefore, a truly comprehensive approach must integrate mindfulness-based stress reduction protocols alongside pharmacological and environmental interventions. The somatic impact of chronic inflammation cannot be divorced from its neuroendocrine underpinnings.
Melanie Taylor
November 26, 2025 AT 18:12So I just tried the saline rinse for the first time… and I almost cried it felt so good 😭 I’ve been using this old neti pot my grandma gave me and I didn’t even know I was using tap water 😳 I’m so scared now but also so hopeful! I bought a sterile bottle and a new kit!! 🙌 I’m gonna post a pic of my new setup tomorrow!! 💪 #SinusFreedom #NetiPotLife