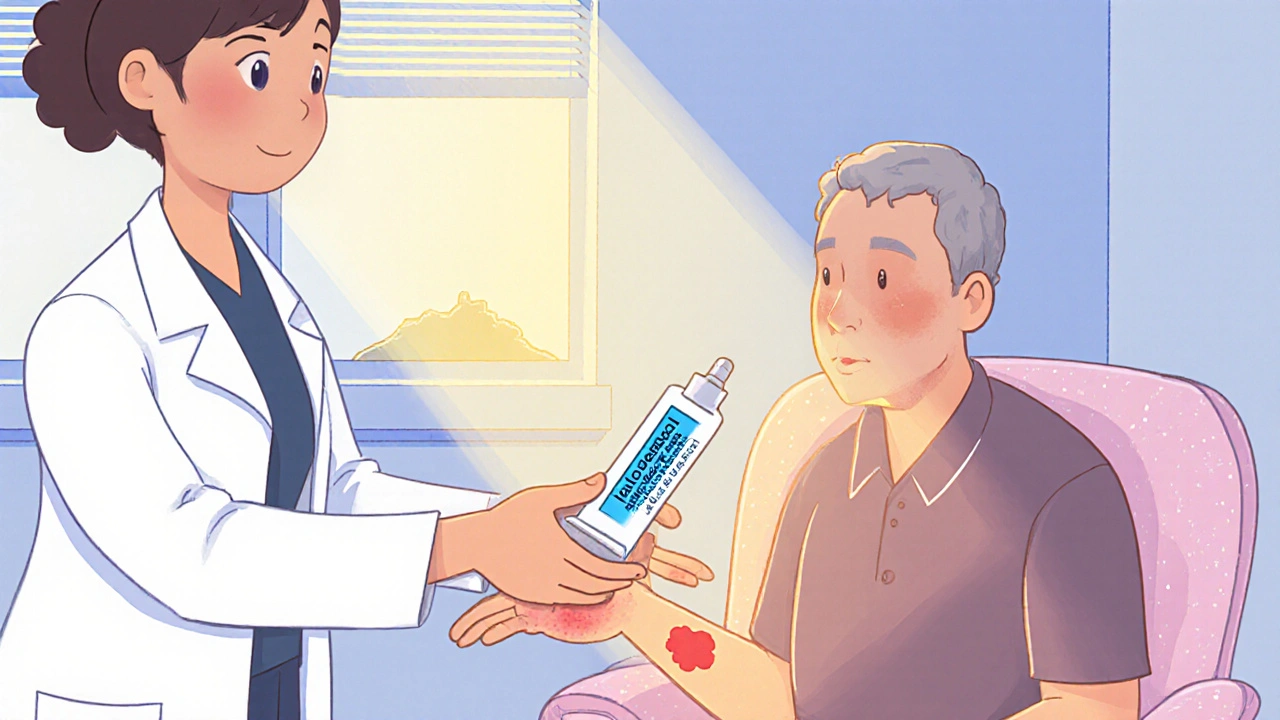
When using Halobetasol a high‑potency topical corticosteroid prescribed for conditions like psoriasis and eczema, many patients worry about side effects such as skin thinning, burning, or hormonal changes. This guide walks you through practical ways to keep those problems at bay and shows what to do if they still show up.
Key Takeaways
- Limit halobetasol to the shortest effective period (usually 2‑4 weeks).
- Combine treatment with a gentle moisturizer to protect the skin barrier.
- Watch for early signs of skin atrophy, burning, or systemic effects and act fast.
- Ask your physician about intermittent‑therapy schedules or lower‑potency alternatives.
- Maintain a simple skin‑care routine: clean, moisturize, protect, and re‑evaluate.
What Is Halobetasol and Why It’s Potent
Halobetasol belongs to the corticosteroid family. It’s classified as a super‑high‑potency (Class I) agent, meaning it delivers a stronger anti‑inflammatory punch than mid‑range steroids like mometasone. Because of that power, it’s typically reserved for stubborn plaques of psoriasis or thick eczema that haven’t responded to milder options.
The drug works by binding to glucocorticoid receptors in skin cells, shutting down inflammatory signals, and reducing immune cell traffic. That rapid suppression is a double‑edged sword: while lesions calm down fast, the same pathway can also thin the skin and, in rare cases, suppress the body’s own cortisol production (the HPA axis).
Typical Side Effects You Might Notice
Even when you follow a doctor’s instructions, halobetasol side effects can sneak in. Below are the most common signals and why they happen:
- Burning or stinging: the steroid can irritate nerve endings, especially on broken or raw skin.
- Dryness and flaking: reduced skin cell turnover makes the surface less supple.
- Skin atrophy (thinning): prolonged collagen breakdown leads to a paper‑thin appearance.
- Stretch marks (striae): weakened dermal fibers can tear under tension.
- Systemic signs: in very high‑dose or extensive‑area use, you might see fatigue, mood swings, or a slight increase in blood sugar because the drug enters the bloodstream.
Spotting any of these early lets you intervene before the problem deepens.
Prevention Checklist - How to Use Halobetasol Safely
- Follow a time‑limit. Most guidelines advise no more than 2‑4 weeks of continuous use, unless a specialist explicitly extends it.
- Apply a thin layer. Use the “finger‑tip amount” (about the size of a pea) for each affected area. Over‑application boosts side‑effect risk without extra benefit.
- Target only lesions. Do not spread the cream over healthy skin. Padding the edges with a bland moisturizer can protect surrounding tissue.
- Combine with a barrier repair. Apply a fragrance‑free, ceramide‑rich moisturizer at least 30 minutes after the steroid has absorbed. This restores lipids and lessens dryness.
- Schedule intermittent breaks. After 2 weeks, pause for a few days to let the skin recover. Many dermatologists recommend a “week‑on, week‑off” pattern for chronic patches.
- Consider lower‑potency alternatives. If the plaque improves quickly, discuss switching to a mid‑strength steroid (e.g., triamcinolone) with your physician.
- Use sunscreen. Halobetasol can make skin more photosensitive. A broad‑spectrum SPF30+ applied each morning reduces the chance of UV‑related damage.
Following this checklist dramatically cuts the odds of a nasty reaction.
Comparison of Common Prevention Strategies
| Strategy | How It Works | Pros | Cons |
|---|---|---|---|
| Limited‑time use (2‑4 weeks) | Reduces cumulative steroid exposure | Strong evidence of lower atrophy risk | May need alternative therapy for long‑term disease |
| Thin‑layer application | Minimizes excess drug on skin surface | Easily self‑monitored | Requires discipline to avoid “just a little more” |
| Moisturizer barrier | Restores lipids, dilutes steroid concentration | Improves comfort and skin health | Additional product cost |
| Intermittent breaks | Allows skin regeneration between courses | Reduces systemic absorption | Potential flare‑up if disease is aggressive |
| Switch to lower‑potency steroid | Maintains anti‑inflammatory effect with less risk | Long‑term safety | May be less effective for thick plaques |
If Side Effects Appear - Management Steps
Even with preventive measures, a reaction can still happen. Here’s a quick action plan:
- Stop the product. Discontinue halobetasol immediately if you notice severe burning, sudden thinning, or systemic symptoms.
- Switch to a bland emollient. Apply a thick, fragrance‑free ointment (e.g., petroleum jelly) to keep the skin moisturized.
- Contact your physician. Ask for a replacement with a milder steroid or a non‑steroidal topical (like calcineurin inhibitors).
- Monitor for systemic signs. If you feel persistent fatigue, unusual weight gain, or mood changes, get blood work to check cortisol levels.
- Consider physical therapy. For skin atrophy causing tightness or reduced mobility, gentle massage can improve circulation.
Prompt response usually reverses early changes. Persistent atrophy may need laser resurfacing or other dermatologic procedures, but those are rare.

Real‑World Example: Sarah’s Journey
Sarah, a 34‑year‑old graphic designer, was prescribed halobetasol for a stubborn plaque on her forearm. She applied it twice daily for three weeks, then noticed a faint red line and a gritty feeling. Following the checklist, she stopped the cream, started a ceramide moisturizer, and booked a quick tele‑visit. Her dermatologist swapped her to a low‑potency steroid and added a week‑off schedule. Within two weeks, the line faded and the skin felt normal again. Sarah’s story underscores how a simple break and barrier repair can save you from bigger problems.
Tips From Dermatology Experts
- Never use halobetasol on the face unless a specialist says it’s safe.
- Avoid occlusion (covering the area with plastic wrap) unless directed-occlusion boosts absorption and side‑effect risk.
- Keep a diary of application dates and any sensations; patterns emerge quickly.
- For large‑area diseases like widespread psoriasis, clinicians often combine a short halobetasol burst with systemic therapy (e.g., biologics) to limit topical exposure.
Frequently Asked Questions
Can I use halobetasol on my scalp?
Scalp skin is thinner, so the risk of irritation and atrophy is higher. Most dermatologists reserve halobetasol for short‑term use on isolated patches and always recommend a low‑potency rinse‑off steroid for broader scalp involvement.
Is it safe to combine halobetasol with a vitamin D analogue?
Yes, many treatment plans pair halobetasol with calcipotriene (a vitamin D analogue) to boost efficacy while allowing a quicker taper of the steroid. Always follow the timing instructions-apply the steroid first, wait 15 minutes, then add the vitamin D cream.
What signs indicate HPA‑axis suppression?
Symptoms can be subtle: chronic fatigue, low blood pressure, unexplained nausea, or difficulty handling stress. Blood tests showing low morning cortisol confirm suppression. If you suspect this, stop the steroid and get a rapid‑acting cortisol replacement under doctor supervision.
How often should I see my dermatologist while using halobetasol?
Schedule a follow‑up after the first two‑week course. If the lesion clears, you can stop or transition to a milder option. For chronic conditions, a quarterly check‑in helps catch early side‑effects.
Can children use halobetasol?
Pediatric use is limited to severe cases and always under specialist supervision. Children’s skin is more permeable, so the treatment duration is usually shorter (often 1‑2 weeks) and the amount applied is strictly measured.




Scott Shubitz
October 15, 2025 AT 17:12Seriously, you think slapping a super‑potent steroid on your skin without a battle plan is a good idea? Halobetasol is a fire‑cracker-use it sparingly or you’ll end up with skin that looks like parchment! Stick to the thin‑layer rule, set timers, and keep that moisturizer handy, or you’ll be the star of your own horror story.
Soumen Bhowmic
October 27, 2025 AT 05:59First and foremost, thank you for compiling such a thorough guide; it serves as a solid foundation for both patients and clinicians alike. By emphasizing the importance of a limited treatment window, you already mitigate a large chunk of the risk associated with Class I steroids. Moreover, incorporating a barrier repair strategy aligns perfectly with the modern “moisturizer‑first” paradigm that dermatology has been advocating for years. It is also worth noting that the “finger‑tip amount” recommendation may vary slightly depending on body surface area, which is an essential nuance for those managing extensive plaques. In practice, I have found that a structured diary, where patients log each application with dates and any sensations, dramatically improves adherence and early detection of side‑effects. Additionally, scheduling intermittent breaks not only allows for skin regeneration but also reduces systemic absorption, a fact that cannot be overstated when treating adolescents. When counseling patients, I always stress that the “week‑on, week‑off” model should be personalized; some individuals may need a shorter break if their disease flares, while others tolerate a longer hiatus without relapse. It is equally critical to educate about the perils of occlusion-covering the treated area with plastic can turn a modest dose into a potent systemic exposure in a matter of hours. The guide’s recommendation to switch to a mid‑potency alternative once improvement is evident is sound, yet it could be expanded to include specific tapering schedules, such as reducing frequency from twice daily to once every other day before discontinuation. I also appreciate the inclusion of sunscreen advice; photosensitivity is often overlooked and can compound skin atrophy when UV damage is added to steroid‑induced thinning. For patients with extensive psoriasis, combining a brief halobetasol burst with a systemic biologic not only limits topical exposure but also provides a synergistic effect, a point that merits explicit mention. Finally, the real‑world example of Sarah underscores the practicality of the checklist, highlighting how prompt action can reverse early atrophic changes. In summary, your checklist is both comprehensive and actionable, but integrating personalized dosing algorithms, diary tools, and clear tapering protocols would make it an even more robust resource for the dermatology community. Furthermore, integrating patient‑reported outcome measures into follow‑up visits can capture subtle changes in skin elasticity that might escape visual inspection. Clinicians should also consider periodic laboratory monitoring for cortisol levels if treatment exceeds four weeks, as this proactive step can catch HPA‑axis suppression before clinical symptoms manifest.
Jenna Michel
November 7, 2025 AT 19:46Hey team-let’s power‑up your skin‑care regimen! 🚀 By leveraging ceramide‑rich emollients, you create a lipid‑fortified shield that synergistically dampens the steroid’s irritant potential; think of it as a nano‑coat protecting dermal collagen. Remember, timing is key-apply the moisturizer at least 30 minutes post‑application to maximize barrier restoration. Stay vigilant, track any tingle or erythema, and you’ll stay ahead of the curve; your skin will thank you!
Abby Richards
November 19, 2025 AT 09:32Great post! 👍 It’s clear, concise, and packed with practical tips. I especially love the reminder to use a “finger‑tip amount” – it prevents over‑application and reduces the risk of atrophy. Keep the advice coming! 😊
Lauren Taylor
November 30, 2025 AT 23:19Thank you for sharing this comprehensive guide; it truly democratizes knowledge that was once confined to specialist clinics. By breaking down the protocol into bite‑size steps, you empower patients from diverse backgrounds to take ownership of their treatment journey. It’s crucial to recognize that skin‑type variability also influences how halobetasol is tolerated, so personalized moisturiser recommendations can bridge that gap. For example, individuals with eczema‑prone skin may benefit from thicker ointments like petrolatum, whereas those with oily skin might prefer lighter, non‑comedogenic creams. Moreover, integrating culturally relevant analogies-such as comparing the “thin‑layer” technique to a chef’s drizzle of sauce-can enhance comprehension across linguistic barriers. Encouraging patients to maintain a simple logbook, perhaps using a smartphone app, further supports adherence and early detection of adverse events. Lastly, fostering an open line of communication with dermatologists ensures that any unexpected flare‑ups are addressed promptly, reinforcing a collaborative care model that respects both medical expertise and patient lived experience.
Vanessa Guimarães
December 12, 2025 AT 13:06Oh, how delightful – another “expert guide” that parrots the same old cautionary tales we’ve been hearing since the dawn of corticosteroids. One would think that a drug as potent as halobetasol warrants more than a checklist of common‑sense steps, yet here we are, patting ourselves on the back for recommending sunscreen. As if the average patient hasn’t already been bombarded with SPF warnings until they develop a rash. Nevertheless, let us all continue to wave the flag of superficial vigilance while ignoring the deeper systemic implications that truly deserve scrutiny.
Lee Llewellyn
December 24, 2025 AT 02:52While I appreciate the intention behind this guide, I can’t help but question its underlying premise-that a topical steroid can ever be truly “safe” when wielded without a grain of skepticism. First, the notion of a “short‑term” 2‑4‑week window is arbitrarily defined; clinicians often extend treatment based on anecdotal success, blurring the line between recommendation and reality. Second, the emphasis on moisturizers, though well‑meaning, borders on the trivial when systemic absorption can still occur through compromised epidermis. Third, the recommendation to “pause for a few days” fails to consider aggressive disease phenotypes that simply rebound with greater vigor during breaks. Moreover, the guide glosses over the fact that many patients are already on systemic immunomodulators, making any added topical potency a potential catalyst for HPA‑axis suppression. Fourth, the reliance on patient‑kept diaries assumes a level of health literacy that is not universally present, especially in underserved communities. Fifth, the table presenting pros and cons seems to oversimplify complex pharmacokinetic dynamics into binary choices, which is misleading at best. Sixth, the occasional mention of “ceramide‑rich moisturizers” neglects the cost barrier for low‑income individuals who cannot afford such products. Seventh, the advice to use sunscreen, while sensible, ignores the reality that many patients already practice inconsistent sun protection. Eighth, the guide’s tone is reassuring, but reassurance without robust evidence can lull patients into complacency. Ninth, the case study of “Sarah” is anecdotal and offers little statistical weight. Lastly, I would advocate for a more critical discourse that challenges the status quo rather than merely reiterating conventional wisdom.
Drew Chislett
January 4, 2026 AT 16:39Really helpful stuff! Keeping the treatment short, using a good moisturizer, and taking breaks can make a big difference. It’s awesome to see such practical advice that lets you stay in control of your skin health. Keep it up!
Rosalee Lance
January 16, 2026 AT 06:26In the grand tapestry of dermatologic care, each thread of caution weaves a pattern of resilience; halobetasol may be a mighty brush, but with mindful strokes, we paint health rather than ruin. Let’s cherish the balance between potency and prudence, for the skin is not merely a canvas but a living narrative.
Kara Lippa
January 27, 2026 AT 20:12Use a thin layer and moisturize daily.
Puneet Kumar
February 8, 2026 AT 09:59Namaste and welcome-this guide bridges both Western dermatology and traditional skin‑care wisdom. By acknowledging that barrier repair is a universal principle, we honor practices ranging from Ayurvedic oil massages to modern ceramide lotions. Tailoring the application schedule to fit cultural routines, such as incorporating the treatment into morning prayers or evening tea time, can improve adherence across diverse populations. Let us celebrate this fusion of knowledge and ensure every patient feels seen.
michael maynard
February 19, 2026 AT 23:46Look, you think a little cream won’t mess you up? Think again-every drop is a tiny time‑bomb waiting to detonate your skin’s integrity. If you’re not logging each dab like a spy tracking a covert mission, you’re practically signing a death‑warrant for your dermal collagen. Don’t be naïve; the “breaks” they suggest are a myth unless you’re willing to watch the flare‑up like a horror film.