
Getting the right dose of medicine for your child isn’t just important-it can be life-saving. Too little and the infection won’t clear. Too much and you could send your child to the emergency room. The good news? Most dosing errors at home are avoidable. The bad news? Almost 7 in 10 parents get it wrong-often because they’re using the wrong tool or misunderstanding the numbers.
Why Milliliters (mL) Are the Only Unit That Matters
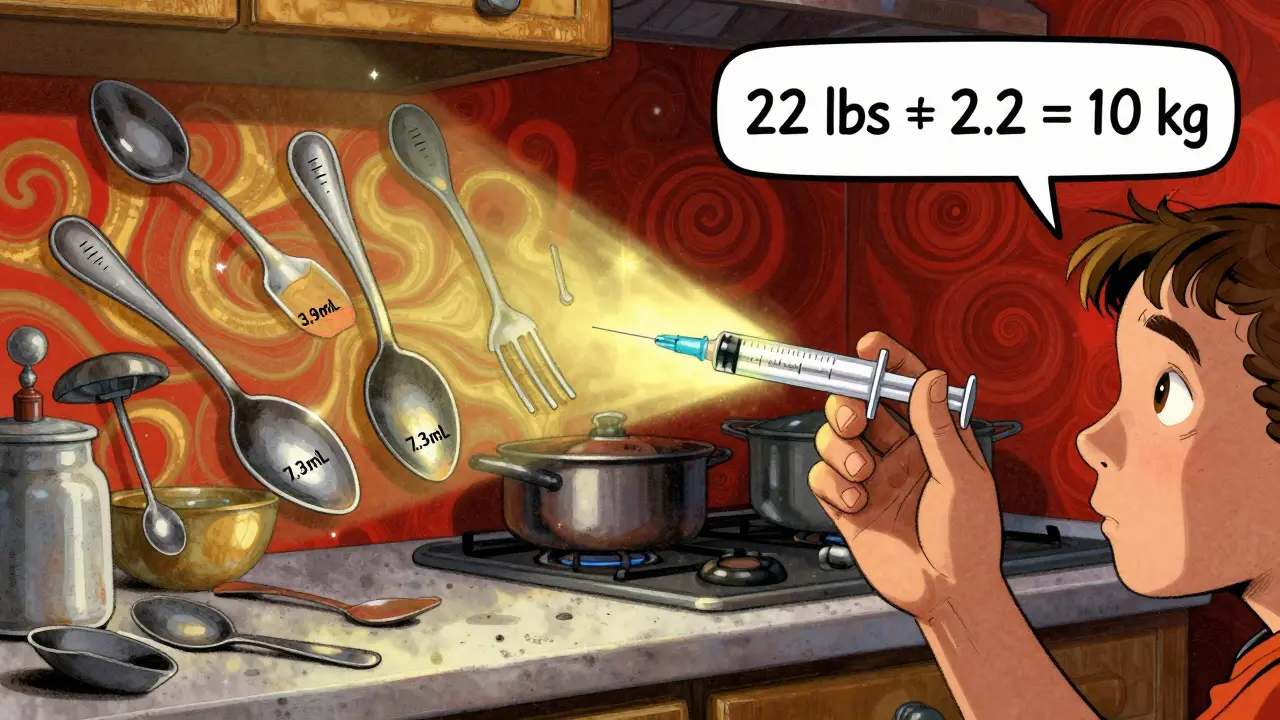
Forget teaspoons and tablespoons. They’re not just inaccurate-they’re dangerous. A kitchen teaspoon can hold anywhere from 3.9 to 7.3 milliliters, depending on how full you pour it. But a standard teaspoon of medicine? That’s supposed to be exactly 5 mL. When you’re giving a child 2.5 mL of amoxicillin, using a regular spoon could mean giving them 1.5 mL too much-or too little. That’s a 60% error.
The CDC, the American Academy of Pediatrics, and the FDA all agree: pediatric liquid medications should only be measured in milliliters (mL). No more tsp, tbsp, or ‘a capful.’ Labels and prescriptions must say mL. If you see ‘teaspoon’ on the bottle, ask the pharmacist to rewrite it. Most pharmacies still mix units-only 57% of prescription labels follow the CDC’s mL-only rule as of 2023. Don’t assume it’s correct. Always double-check.
The Right Tools for the Job
Not all measuring tools are created equal. Here’s what works-and what doesn’t:
- Oral syringes (1-10 mL): The gold standard. They’re accurate, easy to control, and perfect for doses under 5 mL. Studies show they’re 94% accurate. For tiny doses like 0.5 mL or 1.2 mL, they’re the only safe choice.
- Dosing cups (5-30 mL): Fine for older kids who can drink from a cup, but error rates jump to 68.5% for doses under 5 mL. They’re also easy to spill or overfill.
- Droppers: Usually included with infant medications. Good for small volumes, but hard to read precisely. Only use if it’s the only tool provided-and even then, double-check the markings.
- Household spoons: Never use them. A dessert spoon, soup spoon, or coffee spoon? All vary wildly. One study found parents using spoons were 3 times more likely to overdose.
Always use the measuring device that came with the medicine. Don’t swap it out for something you think is ‘easier.’ If you lost the syringe, call the pharmacy. They’ll give you a new one for free.
How to Read an Oral Syringe Correctly
Even with the right tool, mistakes happen. Here’s how to get it right every time:
- Hold the syringe upright. Don’t tilt it. Gravity pulls the liquid down, and if you’re looking at it sideways, you’ll misread the level.
- Look at the meniscus-the curved surface of the liquid. The correct dose is where the bottom of that curve lines up with the mark. Not the top. Not the middle. The bottom.
- Keep your eye level with the measurement. Don’t look down from above or up from below. It’s like reading a ruler-you need to be straight on.
- Double-check the number. Is it 0.5 mL or 5 mL? That’s a tenfold difference. One mistake, one fatal dose. If you’re unsure, ask the pharmacist to show you.
Pro tip: Use a permanent marker to mark the syringe at your child’s most common doses-like 2.5 mL or 5 mL. That way, you’re not guessing every time.
Weight-Based Dosing: Converting Pounds to Kilograms
Many pediatric medications are dosed by weight: mg per kilogram (mg/kg). That means you can’t just guess based on age. You need to know your child’s exact weight in kilograms.
Here’s how to convert: Divide pounds by 2.2.
Example: Your child weighs 22 pounds.
- 22 ÷ 2.2 = 10 kg
If the doctor prescribed 40 mg/kg/day of amoxicillin in two doses, that’s 40 × 10 = 400 mg per day. Split into two doses? That’s 200 mg each.
Now check the concentration: if the bottle says 400 mg per 5 mL, then 200 mg equals 2.5 mL. You’re not guessing-you’re calculating.
Write this down. Keep a small note in your wallet or phone: child’s weight in kg, common doses, and concentrations. It saves stress and prevents errors.
What to Do When Your Child Refuses Medicine
Over two-thirds of parents report their child spits out, coughs, or refuses liquid medicine. It’s normal. But here’s what not to do: don’t mix it into a full bottle of juice or a big bowl of food. That means your child might not get the full dose.
Instead:
- Use a syringe to gently place the medicine in the side of the mouth, near the cheek. Avoid the front-kids spit that out easily.
- Try mixing the dose with a small spoonful (1-2 tsp) of applesauce, pudding, or yogurt. Stir well and give it all at once.
- If the medicine is flavored, ask the pharmacy if they can add a flavor like cherry or bubblegum. Many can.
- Never force it. If your child vomits right after, don’t redose unless the doctor says to. Overdosing is more dangerous than underdosing.
Common Mistakes and How to Avoid Them
Here’s what goes wrong-and how to fix it:
- Mixing up mg and mL: These are totally different. mg is the amount of drug. mL is the volume of liquid. Confusing them causes 36% of pediatric errors. Always read both numbers.
- Not shaking the bottle: Antibiotics and other suspensions settle. If you don’t shake well before each dose, your child gets less medicine. Shake for 10 seconds-like you’re making a cocktail.
- Using old or dirty tools: Residue from previous doses can change the concentration. Rinse the syringe with water after each use. Don’t sterilize it-just wash and air-dry.
- Multiple caregivers using different methods: Grandparents, babysitters, daycare staff-they all need to know the same routine. Write it down. Show them the syringe. Send a photo of the correct dose in your text messages.

What’s New in Pediatric Dosing (2025-2026)
Things are improving. By 2026, the FDA expects nearly all pediatric liquid medications to come with a built-in oral syringe marked only in mL. That’s up from 78% in 2023. Hospitals are already giving them out at discharge.
New tools are coming too:
- Smart dosing cups (coming in 2025): These will beep if you pour too much or too little. Philips Healthcare is testing them in pediatric clinics.
- Color-coded syringes: NurtureShot and Medisana BabyDos use colors to match medication types-blue for antibiotics, red for pain relievers. Studies show they reduce errors by 61%.
- Phone apps: Apps like MedSafety use your phone’s camera to scan the bottle and show you exactly how much to give-with video guides.
These aren’t sci-fi. They’re real, and they’re already helping families.
When to Call the Doctor or Pharmacist
You don’t have to figure this out alone. Call if:
- You’re unsure about the dose-even if it’s just a little off.
- The medicine looks different from last time (color, smell, texture).
- Your child vomits within 15 minutes of taking the dose.
- You accidentally give too much. Don’t wait for symptoms. Call poison control (1-800-222-1222) or your doctor immediately.
Pharmacists are trained for this. They’ve seen every mistake. Don’t be embarrassed to ask. Better to ask twice than risk your child’s health.
Final Checklist Before Giving Medicine
Before you give any liquid medicine to your child, run through this:
- Is the dose written in mL? (If not, ask for it to be rewritten.)
- Do I have the right tool? (Oral syringe for doses under 5 mL.)
- Have I converted the weight to kg? (Pounds ÷ 2.2)
- Have I shaken the bottle? (At least 10 seconds.)
- Am I reading the meniscus at eye level?
- Did I double-check the number? (0.5 mL ≠ 5 mL.)
- Am I giving it to the right child? (Especially important in households with multiple kids.)
It takes less than 30 seconds. But it could save a life.
Can I use a kitchen teaspoon if I don’t have a syringe?
No. Kitchen teaspoons vary from 3.9 to 7.3 mL, while a standard medicine teaspoon is exactly 5 mL. Using one can lead to a 60% overdose or underdose. Always use an oral syringe or the dosing tool that came with the medicine.
What if my child spits out the medicine?
Don’t automatically give another full dose. Wait 15-20 minutes. If they spit out most of it, call your doctor. If they swallowed just a little, it’s usually safe to wait until the next scheduled dose. Overdosing is riskier than underdosing.
Why does the label say both mg and mL?
mg tells you how much active drug is in the dose. mL tells you how much liquid to give. For example, 250 mg/5 mL means every 5 mL of liquid contains 250 mg of medicine. You need both numbers to calculate the right volume.
Are dosing cups ever okay for young kids?
Only for doses over 5 mL and only if your child can drink from the cup without spilling. For any dose under 5 mL-like most antibiotics or fever reducers-oral syringes are safer and more accurate. Dosing cups have a 68.5% error rate at 2.5 mL.
How do I know if I gave the wrong dose?
Signs of overdose include drowsiness, vomiting, rapid heartbeat, or trouble breathing. Signs of underdosing include fever returning, cough worsening, or infection not improving after 48 hours. If you’re unsure, call your doctor or poison control. Don’t wait.





Bradford Beardall
January 10, 2026 AT 10:28Just gave my 2-year-old amoxicillin using the syringe from the pharmacy-no spoon, no guessing. Life changed. I used to wing it with a teaspoon like everyone else until I read this. Now I keep the syringe taped to the fridge with a note: '0.5 mL ≠ 5 mL.' Seriously, if you're using a kitchen spoon, you're playing Russian roulette with your kid's liver.
lisa Bajram
January 10, 2026 AT 23:37OH MY GOSH, YES!!! I just learned this the HARD way-my daughter threw up after I gave her 5 mL thinking it was 0.5 mL because I misread the syringe. I was SO ashamed. But then I started marking my syringe with a Sharpie at 2.5 and 5 mL-and now I feel like a superhero. Also, shaking the bottle like a cocktail? Genius. I do it with flair now. 🙌
Dwayne Dickson
January 12, 2026 AT 07:04It is imperative to underscore the clinical imperative of milliliter-based dosing in pediatric pharmacology. The variance inherent in household utensils constitutes a statistically significant deviation from therapeutic norms, thereby introducing a non-trivial risk of iatrogenic harm. The CDC’s guidelines are not suggestions-they are evidence-based mandates. Failure to comply is not negligence; it is malpractice by omission.
Ted Conerly
January 13, 2026 AT 04:17Don’t overcomplicate this. If you’ve got a kid on liquid meds, get the oral syringe. Keep it with the medicine. Mark it. Shake the bottle. Read the meniscus at eye level. That’s it. No magic. No apps needed. Just do it every time. Your kid’s life isn’t a guess.
Faith Edwards
January 14, 2026 AT 07:27It is profoundly disturbing that so many parents continue to rely on antiquated, unscientific methods for administering life-sustaining medication. The fact that 70% of caregivers commit dosing errors suggests a catastrophic failure of public health literacy. One wonders whether these same individuals also read nutrition labels in binary or use candlesticks to measure time.
Jay Amparo
January 15, 2026 AT 11:39I’m from India and we’ve always used spoons-no one had syringes here. But after reading this, I went to the pharmacy and asked for a free syringe. They gave me two! Now I use it for my daughter’s fever medicine. My mom still uses a spoon but I showed her the video on my phone. She’s starting to listen. Small wins, right?
Lisa Cozad
January 17, 2026 AT 03:34I used to mix meds into juice until I read that you shouldn’t. Now I use a tiny spoon of applesauce-just enough to hide it. My son still makes a face, but he swallows it. And I always write down the dose on my hand with a pen. It’s weird, but it works. No more panic at 2 a.m.
Saumya Roy Chaudhuri
January 18, 2026 AT 18:11You people are overreacting. In my village, we’ve always used teaspoons and never had a problem. My cousin’s kid took amoxicillin for a month with a soup spoon and turned out fine. This is just Western over-medicalization. Stop scaring parents with your ‘meniscus’ nonsense.
anthony martinez
January 20, 2026 AT 04:50Wow. So the FDA is finally doing something right? I thought they just approved candy-flavored opioids for toddlers. Guess I’m wrong. Still, why does it take a 12-page Reddit post to explain how to use a syringe? Someone’s got a lot of explaining to do.
Mario Bros
January 20, 2026 AT 20:23Just bought one of those color-coded syringes-blue for antibiotics, red for Tylenol. It’s like a traffic light for medicine. My 4-year-old even points to the color now. ‘Blue, Mommy, blue!’ It’s cute. And safe. Win-win.
Jake Nunez
January 21, 2026 AT 15:23My grandma used to say, ‘If it’s not hurting them, it’s working.’ She gave my sister a whole tablespoon of cough syrup because ‘it looked right.’ She’s still alive. So maybe this is just fearmongering?
Ian Cheung
January 22, 2026 AT 13:46I used to think the syringe was for cats until I realized it was for my kid. Then I started marking it with a Sharpie. Now I have a whole color-coded system-red for fever, green for antibiotics, yellow for allergies. My wife thinks I’m obsessive. I think she’s one mistake away from an ER visit. We all win when we’re prepared
Christine Milne
January 24, 2026 AT 06:52These guidelines are a product of bureaucratic overreach. In my family, we’ve been using teaspoons since the 1970s. We didn’t have ‘oral syringes’-we had common sense. And we raised three healthy children. Your ‘meniscus’ obsession is a symptom of a society that has lost faith in intuition and replaced it with sterile, clinical rituals.
Kunal Majumder
January 24, 2026 AT 14:06My son hates medicine. I tried everything. Then I found out the pharmacy can flavor it. I asked for bubblegum for his amoxicillin. He took it like candy. No syringe drama. No tears. Just happy kid, happy dad. Sometimes the simplest fix is the best one.