
In 2022, over 107,000 Americans died from drug overdoses. Most involved synthetic opioids like fentanyl. But here’s the good news: you can prepare your family to act fast in an emergency. A simple overdose plan could save a life.
Why Your Family Needs This Plan Now
Every year, drug overdoses claim more lives than car accidents or gun violence in the U.S. According to the CDC Centers for Disease Control and Prevention, 107,941 people died from overdoses in 2022. Synthetic opioids like fentanyl caused 80.1% of those deaths. The critical window between overdose and death is just 4-6 minutes. A family overdose plan turns you from a helpless bystander into a life-saver. It’s not about predicting tragedy-it’s about being ready when seconds count.
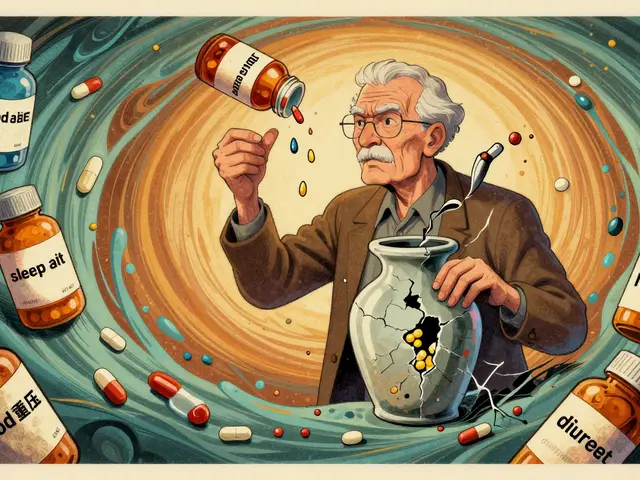
Step 1: Know Your Medications
Start by checking every medicine cabinet in your home. Look for opioid painkillers like oxycodone, hydrocodone, or fentanyl patches. The CDC reports 51.6 million U.S. adults received opioid prescriptions in 2022. Even if you don’t take opioids yourself, someone in your household might. Write down all medications, including dosages and prescribing doctors. Keep this list in a visible spot-like on your fridge or in your wallet. This step alone helps emergency responders act faster if needed.
Step 2: Recognize Overdose Signs
Not all overdoses look the same. The SAMHSA Substance Abuse and Mental Health Services Administration identifies three key signs to watch for: unresponsiveness (can’t wake with shoulder rubs), abnormal breathing (less than 12 breaths per minute), and pinpoint pupils. Fentanyl overdoses move fast-symptoms can appear in just 2-3 minutes. Unlike alcohol or sedative overdoses, opioid overdoses often cause slow, shallow breathing or no breathing at all. Remember: if someone looks "just asleep," check for these signs. Time is everything.

Step 3: Get and Store Naloxone Properly
Naloxone (brand name Narcan) is the life-saving medication for opioid overdoses. The FDA approves two forms: nasal spray (4mg per dose) and injectable. Keep 2-3 doses at home-fentanyl overdoses often need multiple doses. Store naloxone at room temperature (68-77°F), away from direct sunlight. Check expiration dates every 18-24 months. Many pharmacies offer naloxone without a prescription. In 2024, 46 states allow direct pharmacy access. Check CDC or local health departments for free distribution programs. Some cities like New York offer free kits at health centers.
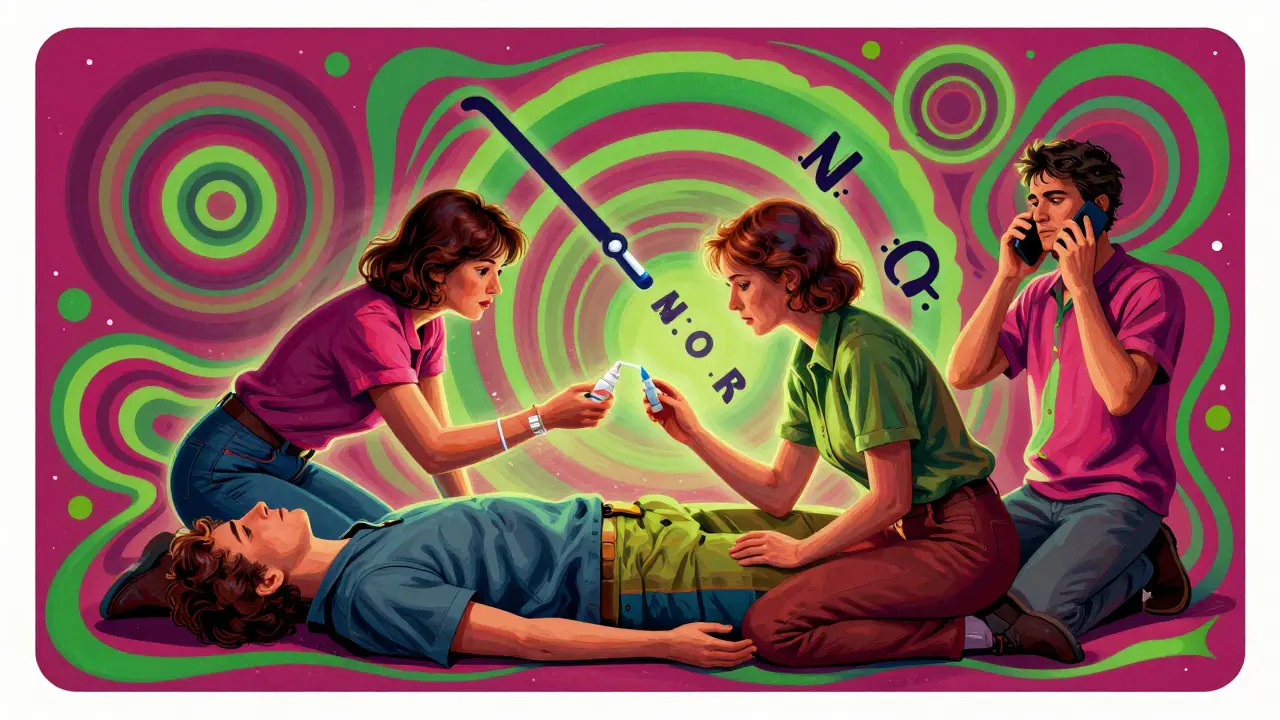
Step 4: Practice the Emergency Steps
Knowing what to do is useless if you don’t practice. Use the A.N.C.H.O.R. Assess, Naloxone, Call 911, Have additional naloxone ready, Observe, Review protocol. First, assess the situation-check breathing and responsiveness. Administer naloxone immediately. Call 911 right away-don’t wait. Keep extra naloxone ready in case the first dose wears off. Watch the person closely for 2-4 hours. Afterward, review what happened to improve next time. Practice with family members, including teens. The American Red Cross offers free 15-minute online courses. Their 2023 study found 89% of participants retained skills after three months.
Step 5: What to Do After Administering Naloxone
Naloxone wears off in 30-90 minutes-but opioids last longer. This means overdose symptoms could return. Stay with the person until EMS arrives. Monitor breathing and keep them awake. If they stop breathing again, give another naloxone dose. The SAMHSA 2023 guidelines stress that "renarcotization" is a real risk. Never leave someone alone after naloxone. Even if they seem fine, they need medical evaluation. This step alone could prevent a second overdose death.
Common Mistakes to Avoid
Many families skip key steps. The Ohio Department of Health found 31% of naloxone kits were expired during overdose incidents. Another 24% had incorrect administration-like not inserting nasal spray deep enough. Some families wait too long to call 911, thinking they can handle it themselves. Remember: Good Samaritan laws protect you in all 50 states. Calling 911 is always the right move. Also, don’t assume naloxone works for non-opioid overdoses. Alcohol or benzodiazepine overdoses need different treatment. Keep your plan simple and specific to opioids.
Frequently Asked Questions
Can naloxone be used for non-opioid overdoses?
No. Naloxone only works on opioids like heroin, fentanyl, or prescription painkillers. It has no effect on overdoses from alcohol, cocaine, or benzodiazepines like Xanax. If you suspect a non-opioid overdose, call 911 immediately and follow emergency instructions.
How long does naloxone last after administration?
Naloxone typically works for 30-90 minutes. However, many opioids last longer in the body. This means overdose symptoms can return after naloxone wears off. Always stay with the person for at least 2-4 hours after administration and call 911 immediately. Never assume one dose is enough.
Where can I get naloxone for free?
Many local health departments and pharmacies offer free naloxone. In 2023, New York City distributed 287,419 free kits through health centers and CVS/Walgreens. Tribal organizations also provide free kits in some regions. Check your state’s health department website or call 211 for local resources. Most states allow pharmacists to dispense naloxone without a prescription.
What if I’m scared to call 911?
All 50 states have Good Samaritan laws protecting people who call 911 during an overdose. These laws prevent arrest for drug possession when seeking help. In 2024, the National Conference of State Legislatures confirmed all states have these protections. Calling 911 is the single most important step to save a life-no matter what.
How often should I check my naloxone kit?
Check expiration dates every 18-24 months. The Washington State Department of Health recommends replacing kits before they expire. Store them properly at room temperature-heat and light can reduce effectiveness. Most pharmacies will replace expired naloxone for free if you bring it in.





AMIT JINDAL
February 6, 2026 AT 10:11Hey y'all, I'm so glad this article came out because honestly, I've been trying to get my family prep'd for years. Like, did you know that fentynal is like 50x stronger than heroin? Yeah, that's insane. And most people don't even realize how common it is. I mean, I checked my medicine cabinet and found a fentynal patch from my grandma's old pain meds. Scary stuff. Anyway, I've got two naloxone kits at home, and I made sure they're stored properly-room temp, no sun. But here's the thing: people always forget to check the expiraton dates. I had one expire last year and almost didn't notice. So please, check yours every 18 months. Also, the signs of overdose-unresponsive, shallow breathing, pinpoint pupils. If you see that, act fast. I practiced with my kids last week, and they were like 'Dad, this is weird' but hey, better safe than sorry. Oh, and don't wait to call 911. I know some folks think they can handle it themselves, but nope. Call 911 first. Good Samaritan laws protect you, so don't worry. I even showed my neighbor how to use the nasal spray. He was like 'Whoa, I never knew it was that easy.' Trust me, this plan is simple but life-saving. My cousin almost died last year, and if we had this knowledge, it might have been different. So yeah, do it. Your family deserves it. 😌
Niel Amstrong Stein
February 6, 2026 AT 10:54Really appreciate the insights shared here. As someone who's traveled a lot, I've seen how different countries handle this. In some places, naloxone is available over the counter, which is awesome. But here in the US, it's still a bit of a hassle. I think the key is education. Like, we need to normalize talking about this stuff. It's not about judging people-it's about saving lives. I've had friends who struggled with addiction, and having this knowledge could have made a huge difference. Also, the 'A.N.C.H.O.R.' method is solid. Practicing it with your family is a great idea. Just remember, it's okay to ask for help. We're all in this together. 🌍❤️
Paula Sa
February 8, 2026 AT 08:07It's heartening to see such a detailed guide. As someone who's worked in healthcare, I believe that preparation is the first step toward saving lives. Every family should have a plan, and this guide makes it so accessible. I've seen too many cases where hesitation cost precious time. But with naloxone and knowledge, we can change that. It's not about fear-it's about empowerment. Let's keep the conversation going and support each other. Together, we can make a difference. 💕
Mary Carroll Allen
February 9, 2026 AT 04:47Paula, you're absolutely right! It's so important to empower families. But wait-did you know that in some states, pharmacists can't dispense naloxone without a prescription? Thats crazy! We need to push for universal access. Also, the signs of overdose aren't always obvious. I had a friend who thought their loved one was just sleeping, but it was an overdose. They almost died. So, let's spread awareness like wildfire. This isn't just a guide-it's a lifeline. Let's make sure everyone knows this. 💪
Joey Gianvincenzi
February 11, 2026 AT 00:23Your assertion regarding pharmacists' ability to dispense naloxone is factually incorrect. In 46 states, as per the CDC's 2024 guidelines, naloxone is available without a prescription. This is a matter of public health policy, and misinformation is detrimental. Furthermore, the term 'lifeline' is hyperbolic; it is a critical tool that requires proper training. I urge you to verify your sources before making such claims. This is not a game; lives are at stake.
Amit Jain
February 12, 2026 AT 22:01Hold on. This whole 'family overdose plan' thing is overhyped. Sure, naloxone is useful, but most overdoses happen to people who don't have families around. Like, if you're using alone, who's gonna save you? Also, the CDC stats are misleading-they count every death as a 'drug overdose' without considering underlying causes. We need to address the root problem: poverty and mental health. Not some checklist for families. This is just fearmongering. 🎭
Sarah B
February 14, 2026 AT 02:51Do it now.
Tola Adedipe
February 15, 2026 AT 22:28I agree with the urgency but disagree with the 'no debate' part. This is a complex issue that needs nuanced solutions. However, I support immediate action. We must ensure naloxone access while also addressing mental health and addiction. Collaboration is key. Let's work together to save lives without demonizing those affected. It's possible to be both aggressive and compassionate.