PHQ-9 Depression Symptom Tracker Calculator
Enter your weekly scores (0-3) for each PHQ-9 item to track your depression symptoms. Scores are based on how often you experienced these symptoms during the past 2 weeks.
When you start taking an antidepressant, you’re not just hoping it works-you’re also bracing for what might come with it. Sleeplessness. Weight gain. Sexual dysfunction. Nausea. These aren’t just side effects listed in fine print; they’re real, daily struggles that can make you question whether the trade-off is worth it. And here’s the hard truth: antidepressant monitoring isn’t happening the way it should. Most patients aren’t being asked to track their symptoms systematically. Providers often rely on vague questions like, “How are you feeling?” after months of treatment. That’s not enough. You need a clearer way to know if the drug is helping-or hurting you more than the depression itself.
Why Tracking Matters More Than You Think
About 30 to 40% of people with depression don’t get better on their first antidepressant. That’s not rare. That’s normal. And it’s not because they’re “not trying hard enough.” It’s because depression doesn’t respond the same way for everyone. What works for one person might do nothing-or make things worse-for another. The key isn’t just changing pills. It’s measuring what’s happening as you take them. That’s where structured monitoring comes in. It’s not a fancy term. It’s simple: write down how you feel, and track your side effects, week after week. Studies show that when patients do this, remission rates jump by 50 to 60%. That’s not a small boost. That’s the difference between still feeling stuck after six months and actually starting to feel like yourself again. The most common tools used by clinicians are the PHQ-9 and the BDI. The PHQ-9 asks nine questions about your mood, sleep, energy, and thoughts over the past two weeks. Each answer is scored 0 to 3. Add them up. A score of 15 or higher means moderate to severe depression. A score below 5? That’s often remission. The BDI is longer-21 questions-but it gives a more detailed picture. Both are backed by decades of research. They’re not guesses. They’re data.What Your Doctor Should Be Asking (But Probably Isn’t)
Most primary care visits last 15 minutes. That’s not enough time to dig into how you’re really doing. But here’s the fix: you don’t have to wait for your doctor to ask. Start tracking yourself. Use the PHQ-9. Print it out. Fill it out every Sunday night. Keep a notebook or use a free app like Moodfit or Sanvello. Record your score. Then write down three things: one thing that felt better this week, one thing that got worse, and one side effect you noticed-like dry mouth, dizziness, or loss of libido. Bring this to your next appointment. Suddenly, your visit isn’t a vague chat. It’s a conversation based on facts. Doctors who use these tools regularly see better outcomes. A 2021 JAMA Network Open study found that patients who tracked their PHQ-9 scores reported 43% higher satisfaction with treatment. Why? Because they weren’t just told to “stick with it.” They had proof-of progress, of setbacks, of side effects that needed attention.Side Effects: The Hidden Cost of Treatment
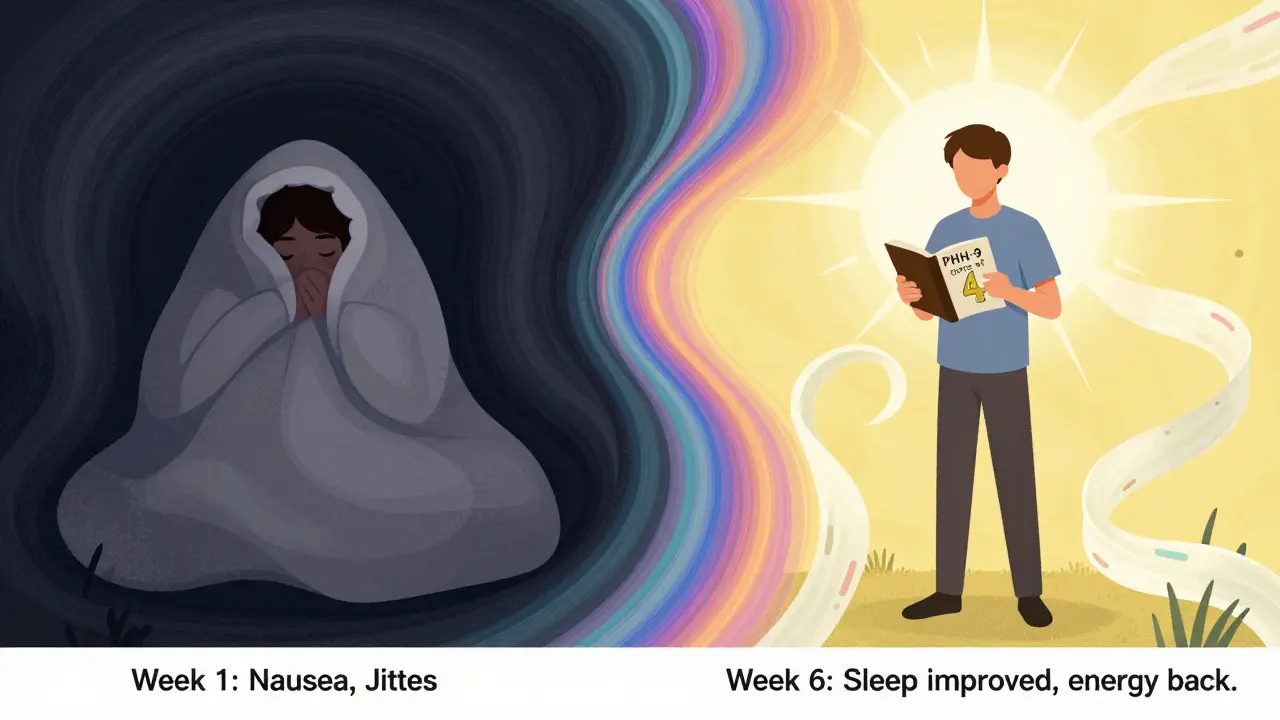
Let’s talk about the side effects nobody wants to admit. Sexual dysfunction is the big one. In one study, 61% of people on SSRIs stopped taking them because their sex life got worse and no one talked about it. That’s not just a side effect-it’s a dealbreaker. And it’s not rare. Up to 74% of people on antidepressants report at least one bothersome side effect. The problem isn’t the drug. It’s the silence around it. If you’re having trouble sleeping, or gaining weight, or feeling emotionally numb, your doctor needs to know. But they can’t fix what they don’t know. The Antidepressant Side-Effect Checklist (ASEC) is a simple tool that lists 15 common side effects. Rate each from 0 (none) to 4 (severe). That’s it. You don’t need a PhD to use it. Just honesty. And here’s something most patients don’t realize: sometimes, side effects fade. Nausea and jitteriness often improve after two to four weeks. But if sexual problems or fatigue stick around past six weeks, that’s a signal. Maybe it’s time to adjust the dose. Maybe switch medications. But you can’t make that call without data.Therapeutic Drug Monitoring: The Science Behind the Dose
You might be taking exactly what your doctor prescribed. But that doesn’t mean your body is processing it the same way as someone else’s. That’s where Therapeutic Drug Monitoring (TDM) comes in. It’s a blood test that measures exactly how much of the drug is in your system. For some people, even the “right” dose is too low. For others, it’s too high. A 2022 meta-analysis found that 50 to 70% of people who don’t respond to antidepressants actually have drug levels below the therapeutic range-even when they’re taking their pills faithfully. TDM isn’t magic. It’s science. It’s especially helpful if you’ve tried two or more meds and nothing worked. It’s also useful if you’re on older drugs like TCAs, which have a narrow safety window. The catch? TDM isn’t routine. It’s used in only 8 to 12% of prescriptions, even though guidelines recommend it for up to 35% of cases. Why? Cost. A single test runs $50 to $150. Labs need expensive machines. But if you’re stuck in treatment-resistant depression, it might be worth asking. Some insurance plans cover it if you’ve tried multiple options.Your Role: Becoming Your Own Advocate
You’re not just a patient. You’re a partner in your care. Here’s how to take charge:- Start with a baseline. Before you even start the med, fill out a PHQ-9. Know where you begin.
- Track weekly. Use a notebook, app, or printable form. Don’t wait for your appointment to remember how you felt last Tuesday.
- Set three personal goals. Not “feel better.” Something specific: “Get out of bed by 8 a.m.,” “Call my mom once a week,” “Walk for 10 minutes without zoning out.” Track progress toward those.
- Don’t ignore side effects. Write them down. Even if they seem small. Dry mouth? Jittery hands? Brain fog? Note them. They matter.
- Bring your data. Don’t say, “I feel worse.” Say, “Last week my PHQ-9 was 18. This week it’s 22. I’ve had constant dry mouth and lost interest in sex for three weeks.” That’s a conversation starter.
What Doesn’t Work-and Why
Digital apps like Moodfit and Sanvello are popular. But don’t assume they’re as reliable as paper scales. Studies show their test-retest reliability hovers around 0.72, while the PHQ-9 scores above 0.85. That means apps can be inconsistent. They’re great for reminders and mood logs-but don’t rely on them for clinical decisions. Use them as a supplement, not a replacement. Also, don’t fall into the trap of thinking “more medication = better.” Sometimes, lowering the dose helps. Sometimes, switching to a different class (like from an SSRI to an NDRI) makes all the difference. But you can’t make those choices without tracking. And you can’t justify them to your doctor without data.The Future Is Here-But You Have to Use It
In January 2024, the FDA cleared the first digital therapeutic for depression: Rejoyn. It’s not a pill. It’s a program that requires you to complete a PHQ-9 every week. If you skip it, your clinician gets flagged. It’s not about surveillance. It’s about accountability. And it works. Meanwhile, pharmacogenetic testing-like GeneSight-is becoming more common. These tests analyze your genes to predict how you’ll metabolize certain antidepressants. A 2023 study showed they cut side effects by 30% and improved response rates by 20%. That’s huge. But again, it’s only useful if you’re already tracking your symptoms. The bottom line? Monitoring isn’t optional anymore. It’s the standard. The American Psychiatric Association updated its guidelines in June 2024 to say: systematic monitoring of both efficacy and side effects is required at all stages of treatment. That means if your provider isn’t doing it, they’re falling behind.What to Do Next
You don’t need a fancy app. You don’t need a blood test. You just need to start writing. 1. Go to the PHQ-9 website (it’s free, no login needed). Print it. 2. Fill it out today. Write down your score. 3. Next week, do it again. Compare. 4. Start a side effect log. One line per day: “Dizziness after lunch,” “No energy to shower,” “Sex drive gone.” 5. Bring both to your next appointment. That’s it. No magic. No cost. Just clarity.How long should I wait before deciding if my antidepressant is working?
Most antidepressants take 4 to 6 weeks to show noticeable effects. By week 6, you should see at least a 50% reduction in your PHQ-9 or BDI score if the medication is working. If there’s no improvement by then, talk to your provider about adjusting the dose or switching. Don’t wait longer than 8 weeks without a change-delaying action can make recovery harder.
Can I stop taking my antidepressant if the side effects are too bad?
Never stop abruptly. Even if side effects feel unbearable, contact your provider first. Stopping suddenly can cause withdrawal symptoms like dizziness, nausea, or electric-shock sensations. Your doctor can help you taper safely. In some cases, switching to a different medication with fewer side effects is possible-like moving from an SSRI to bupropion, which is less likely to affect sexual function.
Is tracking my mood really necessary if I feel fine?
Yes. Depression doesn’t always show up as sadness. Sometimes, it’s just numbness, fatigue, or losing interest in things you used to enjoy. You might think you’re “fine,” but your PHQ-9 score could still be in the moderate or severe range. Tracking helps catch subtle changes before they spiral. It also helps you recognize real progress-even if it feels slow.
Why do some people need blood tests for antidepressants?
Blood tests measure how much of the drug is in your system. Some people metabolize medications faster or slower than average. That means even a “standard” dose might be too low or too high for them. This is especially common with older antidepressants like amitriptyline or nortriptyline. Blood tests are most helpful if you’ve tried multiple meds without success, or if side effects are severe despite low doses.
Are apps like Moodfit reliable for tracking depression symptoms?
Apps are useful for daily logging and reminders, but they’re not as accurate as paper-based scales like the PHQ-9. Studies show their consistency is around 0.72, while PHQ-9 has a reliability of 0.85+. Use apps to stay consistent, but print and complete the official PHQ-9 every 2-4 weeks for clinical accuracy. Don’t let app scores replace professional assessment.




Joseph Charles Colin
February 7, 2026 AT 16:04Structured monitoring isn't just a suggestion-it's a clinical imperative. The PHQ-9 has a Cronbach's alpha of 0.86, which means it's psychometrically robust. When patients track weekly, you're not just anecdoting-you're generating longitudinal data that correlates with remission rates above 60% in RCTs. The FDA's clearance of Rejoyn confirms this: objective metrics > subjective self-report. And let's not forget the ASEK: 15-item, Likert-scaled, validated since 2017. If your provider isn't using this, they're practicing in the analog era.
John Sonnenberg
February 8, 2026 AT 18:16Everyone's so obsessed with tracking they forget the real issue: pharmaceutical companies design these drugs knowing full well the side effects are unacceptable-they just count on patients being too exhausted to quit.
Joshua Smith
February 9, 2026 AT 10:20I've been using the PHQ-9 weekly for 8 months now. It's not glamorous, but seeing my score drop from 21 to 6 gave me something concrete to hold onto. I also started the ASEK checklist-dry mouth and brain fog were way worse than I realized. Small changes, big impact.
Jessica Klaar
February 9, 2026 AT 21:51As someone from a community where mental health is still stigmatized, I can't stress enough how powerful simple tools like these are. My mom didn't believe antidepressants worked until I showed her my printed scores. Now she asks me to track every week. It's not just medicine-it's communication.
PAUL MCQUEEN
February 11, 2026 AT 13:18Yeah, right. Track your mood. Bring a notebook. What's next? Are we gonna start journaling our dreams to the FDA? This whole thing feels like a corporate wellness program dressed up as science. I've been on three different SSRIs. None of them helped. And no, I don't want to fill out another damn form.
glenn mendoza
February 13, 2026 AT 07:50It is with profound respect for the scientific rigor of evidence-based psychiatry that I acknowledge the imperative for systematic, quantifiable, and longitudinal patient self-monitoring. The data presented herein is not merely anecdotal-it is statistically significant, peer-reviewed, and aligned with the most recent American Psychiatric Association guidelines. One cannot overstate the ethical obligation to employ such tools.
Kathryn Lenn
February 15, 2026 AT 05:10Let's be real-the entire system is rigged. The PHQ-9? Designed by Big Pharma to keep you compliant. TDM? Only available if you're rich enough to fight your insurance. And don't get me started on Rejoyn-how convenient that the FDA 'cleared' it right after the last big lawsuit. They don't want you better. They want you tracked. Forever.
John Watts
February 16, 2026 AT 23:14You're not alone in this. I started tracking after hitting rock bottom last year. Didn't feel like a person for months. But writing down 'walked to mailbox' and 'ate one meal'-those tiny wins? They added up. You don't need a fancy app. You just need to write one line. One line a week changes everything. You got this.
Randy Harkins
February 18, 2026 AT 16:44Thank you for sharing this. I've been using Moodfit, but after reading this, I switched to printing the PHQ-9 every Sunday. My score went from 19 to 11 in 4 weeks. Also started the ASEK checklist-turns out my 'just tired' was actually sexual dysfunction (scored 3/4). My doctor was shocked. We adjusted my dose. I feel like me again. 🙏
Tori Thenazi
February 19, 2026 AT 04:15So... you're telling me that if I just write down that I 'can't get hard' or 'feel like a zombie' on paper, my doctor will magically fix it? And they won't just push me to another pill? Please. They're not listening. They're just collecting data points for their quarterly KPIs. This isn't care-it's surveillance with a side of placebo.
Monica Warnick
February 19, 2026 AT 13:09My therapist said to track my mood. I did. For six months. I wrote 'nothing changed' every week. I still cried every night. The PHQ-9 didn't help. The ASEK didn't help. The blood test showed I was in range. But I still felt like I was drowning. Maybe the problem isn't the tracking. Maybe it's that no one knows what to do with the data.
Chelsea Deflyss
February 21, 2026 AT 08:00you shoudl be usin the bdi not the phq-9 its way more accuarte and if u dont have time to print it just use the app its fine
Alex Ogle
February 23, 2026 AT 01:30I used to think this was all bullshit. Then I started writing down one thing each day: 'Slept 3 hours,' 'Didn't shower,' 'Cried in the grocery store.' Six weeks in, I looked back and realized I hadn't cried in public in two weeks. I didn't even notice. That's the power of this stuff. It doesn't fix you. But it makes you see the invisible changes. And sometimes… that's enough to keep going.